When you take a blood thinner, you’re managing a delicate balance. These medications save lives by stopping dangerous clots from forming - but if you take too much, they can start bleeding inside your body without warning. And that’s not something you can wait on. Internal bleeding from a blood thinner overdose doesn’t always come with a loud alarm. Sometimes, it starts quietly - a dark stool, a bruise that won’t fade, a nosebleed that won’t stop. By the time you feel weak or dizzy, it’s already serious. Knowing what to do in those first critical minutes can mean the difference between life and death.
What Happens When You Overdose on a Blood Thinner?
Blood thinners like warfarin, apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa) work by slowing down your blood’s ability to clot. That’s good when you have atrial fibrillation or a history of clots. But if you take too much - whether by accident, misreading the label, or taking an extra pill - your blood loses its ability to seal even tiny leaks. That’s when internal bleeding begins.
Warfarin, the oldest of these drugs, takes hours to show its full effect. Even if you took an overdose 12 hours ago, your INR (a blood test that measures clotting time) might still be rising. For newer drugs like apixaban or rivaroxaban, the effects hit faster - sometimes within 2 to 4 hours - but they also wear off quicker. Still, that doesn’t mean you’re safe. A single extra pill can push your INR past 8.0, which is more than double the safe range for most people.
The body doesn’t always scream when something’s wrong. You might feel fine until you notice your urine is pink. Or your stool looks like tar. Or you’ve got a headache that won’t go away - not from stress, but because blood is leaking slowly into your brain. These aren’t normal. They’re red flags.
Signs of Internal Bleeding You Can’t Ignore
Here’s what real internal bleeding looks like, based on emergency room reports and patient stories:
- Black, tarry, or bloody stools - this means bleeding in your stomach or intestines
- Pink, red, or dark brown urine - blood in your kidneys or bladder
- Vomiting blood or material that looks like coffee grounds - upper GI bleeding
- Coughing or spitting up blood - bleeding in your lungs or airways
- Unexplained bruising, especially large patches or spots under the skin (petechiae)
- Prolonged bleeding from minor cuts - more than 10 minutes of pressure doesn’t stop it
- Heavy menstrual bleeding - far beyond your normal flow
- Sudden, severe headache, dizziness, confusion, or vision changes - possible brain bleed
- Swelling, pain, or warmth in your legs - could be a clot turning into a bleed
- Extreme fatigue, pale skin, or shortness of breath - signs your body is losing too much blood
One patient in Sydney told her doctor she thought her dark stools were from eating beets. By the time she got to the hospital, her hemoglobin had dropped to 6.2 g/dL - normal is 12-16. She needed a blood transfusion. That’s not rare. In fact, 28% of people who end up in the ER with a blood thinner overdose waited more than 12 hours before seeking help. They thought it was just a bad stomach bug.

What to Do Right Now - Step by Step
If you or someone you know has taken too much of a blood thinner and shows any of the signs above, don’t wait. Don’t call your pharmacy. Don’t check your phone for symptoms. Call emergency services immediately.
- Call 000 (Australia) or 911 (US) right away. Say: “I think I’ve overdosed on a blood thinner and I’m bleeding internally.” Be specific. Mention the drug name if you know it - warfarin, Eliquis, Xarelto, etc.
- Do NOT take another dose. Even if you think you missed one, don’t double up. This is not a missed pill situation - this is an emergency.
- Write down what you took. The exact name of the drug, how many pills, and when you took them. This saves critical minutes at the hospital.
- Do NOT take aspirin, ibuprofen, naproxen, or any NSAID. These make bleeding worse. Even a single tablet can push you over the edge.
- If you’re bleeding externally, apply firm pressure. Use a clean cloth or bandage. Keep pressure on for at least 10 minutes without checking. Lifting it too soon stops clotting.
- Lie down and elevate the bleeding area. If it’s a leg or arm, raise it above your heart. If you’re dizzy, lie flat. Don’t sit up or stand.
- Bring your medication bottles to the hospital. Even empty ones. The ER staff needs to know exactly what you’ve been taking.
Some people try to “wait it out” because they’re scared of the hospital. But delaying care by even an hour can double your risk of death. A 2022 study found that patients who reached the ER within 2 hours of symptoms had a 97% survival rate. Those who waited 6 hours or more? Only 76% made it.
How Hospitals Treat Blood Thinner Overdose
Once you’re in the ER, the team will act fast. First, they’ll check your INR - that’s the number that tells them how thin your blood is. Normal is 1.0. For most people on warfarin, it’s kept between 2.0 and 3.0. If your INR is over 4.5, you’re in danger. Over 8.0? That’s life-threatening.
Here’s what happens next, depending on the drug:
- For warfarin: If you’re bleeding, they’ll give you 4-factor Prothrombin Complex Concentrate (PCC) - a concentrated dose of clotting factors that works in minutes. They’ll also give you vitamin K (10 mg IV) to help your body start making clotting proteins again. This can take hours to days to fully work, so you’ll be monitored for days.
- For dabigatran (Pradaxa): They’ll use idarucizumab (Praxbind), a specific antidote that reverses the drug in under 10 minutes. It costs around $7,000 per dose, but it’s life-saving.
- For apixaban or rivaroxaban: Andexanet alfa (Andexxa) is the reversal agent. It’s not always in stock, but hospitals with stroke or cardiac units usually keep it.
- If the overdose was recent (under 1 hour): They might give you activated charcoal to soak up any unabsorbed pills in your stomach. But after that? It’s useless.
For some patients - especially those who took a very large overdose but aren’t bleeding yet - doctors may just give vitamin K and watch closely. But that’s rare. Most cases need immediate reversal.
What You Can Do to Prevent This
Most overdoses aren’t intentional. They happen because:
- You forgot if you took your pill and took another
- You switched brands and didn’t realize the dose changed
- You took a new medicine that interacted with your blood thinner
- You drank alcohol or ate too much vitamin K-rich food (like kale or spinach) without adjusting your dose
Here’s how to protect yourself:
- Use a pill organizer with days and times clearly marked
- Set two alarms on your phone - one for morning, one for evening
- Keep a small card in your wallet that says: “On blood thinner - emergency contact and drug name”
- Get your INR checked regularly - weekly at first, then monthly if stable
- Use a home INR monitor if your doctor recommends it - they cost $200-$300 and reduce bleeding risk by 34%
- Never start a new medication (even OTC) without asking your doctor if it interacts with your blood thinner
- Know your HAS-BLED score - if you’re over 65, have high blood pressure, drink alcohol, or have kidney issues, your risk is higher
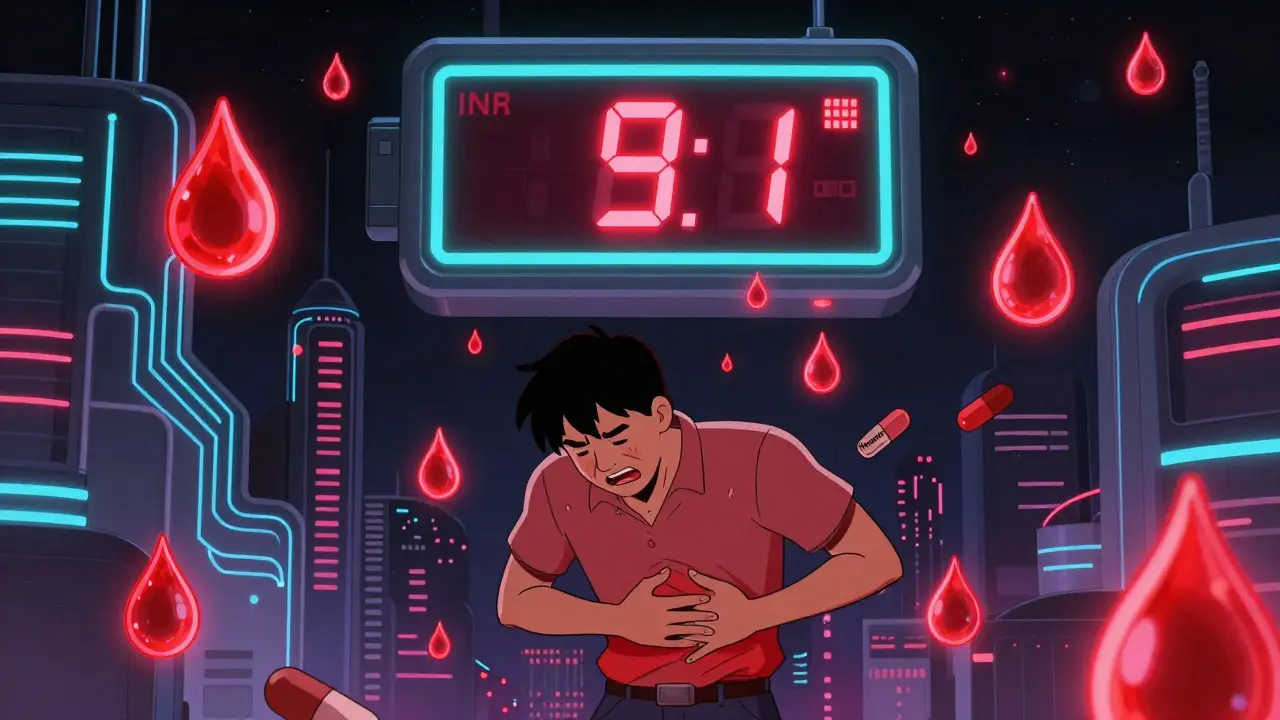
One man in Melbourne used a pill box with alarms. He took his warfarin every night at 8 p.m. One night, his alarm didn’t go off. He didn’t take it. The next night, he took two. He didn’t feel sick. He didn’t think anything of it. Three days later, he passed out in the shower. His INR was 9.1. He spent 11 days in hospital. He’s alive now. He says the alarm system saved him - and he wishes he’d had it sooner.
What Happens After the Emergency?
Surviving an overdose doesn’t mean you’re done. You’ll need close follow-up. Your doctor will adjust your dose, possibly switch you to a different blood thinner, or change how often you get tested. You might need to avoid certain foods, alcohol, or supplements. You’ll also be screened for the root cause - was it a memory issue? A vision problem? A pharmacy error?
Many patients are offered home nursing visits or telehealth check-ins. Some get connected to anticoagulation clinics - specialized teams that manage your meds, test your INR, and answer questions 24/7. Don’t see this as punishment. See it as protection.
And remember - this isn’t your fault. Blood thinners are powerful, complex, and hard to manage. The system isn’t perfect. But you can be smarter about it. And that’s what saves lives.
Can I reverse a blood thinner overdose at home?
No. There is no safe or effective way to reverse a blood thinner overdose at home. Vitamin K for warfarin takes hours to work and must be given under medical supervision. Reversal agents like idarucizumab or andexanet alfa are only available in hospitals. Trying to manage this yourself can lead to fatal bleeding. Call emergency services immediately if you suspect an overdose.
Is it safe to take aspirin if I’m on a blood thinner?
No. Aspirin, ibuprofen, naproxen, and other NSAIDs increase bleeding risk when combined with blood thinners. Even low-dose aspirin can be dangerous. Always check with your doctor before taking any pain reliever. Use acetaminophen (paracetamol) only if approved by your provider.
How long does it take for a blood thinner to leave the body?
It depends on the drug. Warfarin lasts 36-42 hours, but its effect on clotting can last up to 5 days. Newer drugs like apixaban and rivaroxaban wear off faster - about 12-17 hours - but their effects can still linger for 24-48 hours. That’s why even a single extra dose can be dangerous. Never assume the drug is “out of your system” just because it’s been a day.
Can I still take blood thinners after an overdose?
Yes - but only under strict medical supervision. Many people go back on blood thinners after recovery, often at a lower dose or with a different drug. Your doctor will reassess your risk for clots versus bleeding. Some patients switch from warfarin to a DOAC for easier management. Never restart without your doctor’s guidance.
What should I tell the ER staff when I arrive?
Tell them: 1) The name of the blood thinner you took, 2) The exact number of pills you took, 3) The time you took them, 4) Any symptoms you’re having, and 5) Your most recent INR result if you have it. Bring your medication bottles. This saves time and helps them choose the right treatment faster.
Are newer blood thinners safer than warfarin?
They’re easier to manage - no regular INR tests, fewer food interactions - but they’re not safer in overdose. They still cause serious bleeding. The big advantage is that specific reversal agents exist for most of them, which can act faster than vitamin K. But if you don’t get to the hospital quickly, they’re just as dangerous.
Can I drink alcohol while on blood thinners?
Moderate alcohol (one drink a day) is usually okay, but heavy drinking increases bleeding risk and can interfere with how your liver processes the drug. It can also make your INR swing wildly. If you drink regularly, tell your doctor - you may need more frequent testing.

Kayleigh Campbell
December 15, 2025 AT 08:21Elizabeth Bauman
December 16, 2025 AT 23:44Kitty Price
December 18, 2025 AT 14:08James Rayner
December 18, 2025 AT 14:19Andrew Sychev
December 18, 2025 AT 20:59Dylan Smith
December 18, 2025 AT 22:55Kayleigh Campbell
December 20, 2025 AT 17:59Josias Ariel Mahlangu
December 21, 2025 AT 13:21Ron Williams
December 21, 2025 AT 14:00Mike Smith
December 22, 2025 AT 22:34Souhardya Paul
December 23, 2025 AT 14:46