Liver Enzyme Response Calculator
What Your Liver Enzyme Levels Mean
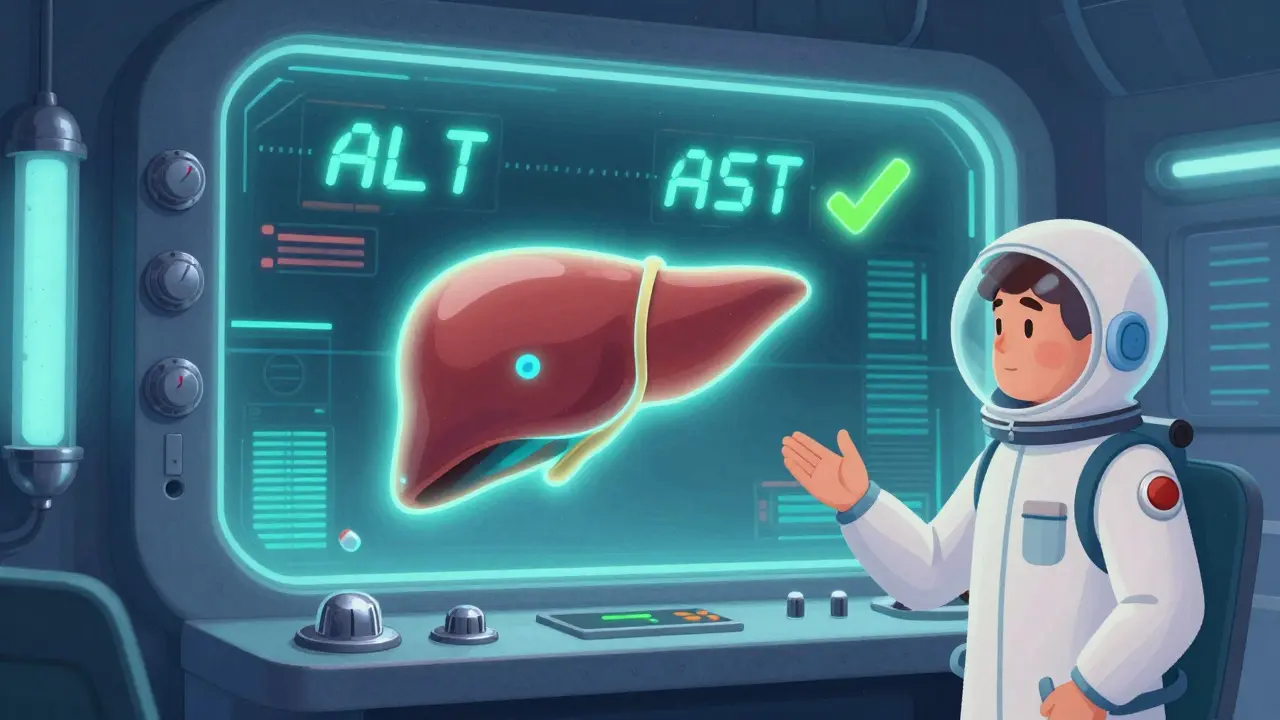
This tool helps you understand what your liver enzyme results mean when taking statins. It's based on the latest medical guidelines from the FDA and major medical societies.
Note: The Upper Limit of Normal (ULN) for ALT and AST is typically 40-50 U/L, but varies by lab. This tool uses 40 U/L as the baseline.
Enter your ALT and AST values to see what action to take.
When you start taking a statin, your doctor might tell you to get a blood test before you begin. That’s usually to check your liver enzymes-ALT and AST. Then, if you’re lucky, you never hear about them again. But if those numbers creep up, it can send panic through your mind. Statin-related liver problems sound scary. Is your liver failing? Should you stop the pill? The truth is, most of the time, it’s not a problem at all.
What Does It Mean When Liver Enzymes Go Up?
ALT and AST are proteins found in liver cells. When those cells get stressed or damaged, they leak these enzymes into your blood. That’s what shows up on a blood test. High levels don’t mean your liver is ruined. They just mean something’s happening inside it. For statins, this happens in about 0.5% to 2% of people. Most of those cases are mild-just a little above normal-and cause zero symptoms.
The FDA says serious liver injury from statins is extremely rare-less than 1 in 10,000 people. Between 1990 and 2020, only 32 confirmed cases of statin-induced liver failure were reported across 20 million patient-years. That’s less likely than being struck by lightning. Yet, people still quit statins over this.
Why Do Statins Affect Liver Enzymes?
It’s not about toxicity in the way most people think. Statins work by blocking an enzyme your liver uses to make cholesterol. But that same enzyme is also involved in making other important molecules, like coenzyme Q10 and certain proteins that help mitochondria-your cells’ energy factories-run smoothly.
Lipophilic statins like simvastatin and atorvastatin slip easily into liver cells. Once inside, they can interfere with mitochondrial function, causing a small increase in oxidative stress. Think of it like revving a car engine too hard for too long. The engine doesn’t break, but it gets hotter. Your liver cells react by releasing a bit more ALT and AST. Hydrophilic statins like pravastatin and rosuvastatin don’t penetrate liver cells as deeply, so they cause fewer enzyme spikes.
Genetics also play a role. If you have a variant in the SLCO1B1 gene, your liver can’t clear statins as efficiently. That increases your chance of enzyme elevation by over three times. It’s not common, but it’s real. And that’s why new genetic tests are starting to appear-though they’re not needed for everyone.
When Should You Worry?
Not every elevated enzyme is a red flag. Doctors look at the number:
- Up to 1.5x the upper limit of normal (ULN): No action needed. Keep taking the statin.
- 1.5x to 3x ULN: Monitor. Retest in 4-6 weeks. Don’t stop the medication unless symptoms appear.
- Above 3x ULN: Pause the statin. Recheck in 1-2 weeks. If it drops, you can often restart safely.
Here’s the kicker: 80% of people with ALT levels between 1-3x ULN never have another issue. Their numbers go back to normal on their own-even if they keep taking the statin. Stopping it unnecessarily is the real risk.
A 2022 Mayo Clinic study tracked 17 patients who stopped their statins because of mild enzyme elevations. Five of them had a heart attack or stroke within 18 months. That’s not coincidence. It’s consequence.
What Else Could Be Raising Your Liver Enzymes?
Before you blame the statin, look elsewhere. In fact, most elevated liver enzymes in statin users aren’t caused by the drug at all.
- Nonalcoholic fatty liver disease (NAFLD): Affects nearly half of adults in Western countries. Surprisingly, people with NAFLD have lower rates of statin-related enzyme spikes.
- Alcohol use: Even moderate drinking can raise ALT. One drink a night? That’s enough.
- Viral hepatitis: Hepatitis B and C are common but often undiagnosed. A simple blood test can rule them out.
- Obesity: Fat around the liver causes inflammation. That’s a major cause of high enzymes.
- Other medications: Painkillers like acetaminophen, antibiotics, or even herbal supplements like kava or green tea extract can do it.
A VA Healthcare study found that when doctors used a checklist to rule out these causes first, unnecessary statin stops dropped by 63%. That’s huge. Don’t assume the statin is the villain.
Who’s at Higher Risk?
Some people are more likely to see enzyme changes:
- People over 75
- Those with kidney disease (creatinine clearance under 30 mL/min)
- People on high-dose statins (80mg atorvastatin, 40mg rosuvastatin)
- Those taking statins with drugs that slow their breakdown-like clarithromycin, cyclosporine, or grapefruit juice
But here’s something surprising: people with existing liver disease, like compensated cirrhosis (Child-Pugh A), can safely take statins. A 2024 European study showed only a 1.3% rate of enzyme spikes above 3x ULN in these patients-almost the same as healthy people. Statins are not banned in liver disease. They’re often recommended.
What Should You Do If Your Enzymes Are High?
Don’t panic. Don’t quit. Do this:
- Check if you have symptoms: yellow skin, dark urine, belly pain, extreme fatigue. If yes, call your doctor immediately.
- If no symptoms and enzyme level is under 3x ULN: Keep taking your statin. Schedule a repeat blood test in 4-6 weeks.
- If it’s above 3x ULN: Stop the statin for 1-2 weeks. Retest. If it drops, your doctor may try a different statin-pravastatin or fluvastatin often work well.
- Get tested for other causes: Hepatitis B/C, alcohol use, NAFLD, and other meds.
Switching statins works in about 70% of cases. One Reddit user saw his ALT jump from 28 to 142 after starting atorvastatin. After switching to pravastatin, his levels dropped back to normal. He’s still on statins two years later. No heart attack. No liver damage. Just a smarter choice.
Why Do So Many Doctors Still Order Routine Liver Tests?
The FDA removed the recommendation for routine liver enzyme testing in 2012. The evidence was clear: monitoring didn’t catch serious problems early. It just caused unnecessary anxiety and stopped people from taking lifesaving drugs.
Yet, a 2023 study found that 35% of primary care doctors still order liver tests every 6 months. That’s over $1.2 billion a year spent on tests that don’t help. It’s not that doctors are wrong-they’re just stuck in old habits. Patients ask. Clinics bill. It’s easier to order the test than explain why it’s not needed.
But you can change that. Ask your doctor: “Is this test really necessary? What will you do if it’s high?” If they say, “We’ll stop the statin,” push back. Say, “I’ve read that mild elevations are common and not dangerous. Can we just retest in a month instead?”
Is There a Better Way?
Yes. New research is looking at supplements like coenzyme Q10. In a phase II trial, taking 100mg daily reduced statin-related ALT elevations by over 40%. It’s not a magic fix, but it might help if you’re prone to this. Still, no one knows if it improves long-term heart outcomes.
Fixed-dose combinations like Vytorin (simvastatin + ezetimibe) are marketed as gentler on the liver. But trials show no real difference in enzyme spikes compared to statins alone. The benefit is lower doses, not better liver safety.
The real solution? Use the lowest effective dose. For most people, 10-20mg of atorvastatin or 5-10mg of rosuvastatin is enough. Higher doses don’t add much benefit but do increase side effect risk.
The Big Picture: Benefits vs. Risks
For every 1,000 people taking a statin for five years:
- 39 will avoid a heart attack or stroke.
- 1 will have a serious liver problem.
- Less than 1 in 10,000 will have liver failure.
That’s not a gamble. That’s a win. Statins are the most studied drugs in history. Their benefits are rock-solid. The liver risk? Mostly noise.
Statin-related liver enzyme elevations are a red herring. They’re a statistical blip, not a medical emergency. If your numbers go up, don’t assume the worst. Talk to your doctor. Rule out other causes. Re-test. Stay on the medication unless you have symptoms or your doctor says otherwise.
Your heart will thank you.
Can statins cause permanent liver damage?
No. Statins do not cause permanent liver damage in the vast majority of cases. Even when liver enzymes rise above three times the normal level, the changes are almost always reversible. Once the statin is stopped or switched, enzyme levels return to normal within weeks. There is no evidence that statins lead to chronic liver disease, cirrhosis, or fibrosis.
Should I stop my statin if my liver enzymes are high?
Only if your ALT or AST is more than three times the upper limit of normal and you have symptoms like jaundice or severe fatigue. For mild elevations-under 3x ULN-you should keep taking the statin. Stopping it increases your risk of heart attack or stroke more than continuing it increases liver risk. Always retest in 4-6 weeks before making any changes.
Which statin is safest for the liver?
Pravastatin and rosuvastatin have the lowest risk of liver enzyme elevation. They are hydrophilic, meaning they don’t penetrate liver cells as deeply as lipophilic statins like simvastatin or atorvastatin. Studies show pravastatin causes enzyme spikes in only 0.3% of users, compared to up to 2% with higher-dose simvastatin. If you’ve had a problem before, switching to one of these is often the best move.
Does having fatty liver mean I can’t take statins?
No. People with nonalcoholic fatty liver disease (NAFLD) actually have a lower risk of statin-induced liver enzyme spikes than those without it. Statins may even help reduce liver fat over time. Major guidelines from the American Gastroenterological Association say NAFLD is not a reason to avoid statins. In fact, statins are often recommended for people with fatty liver who also have high cholesterol.
How often should liver tests be done on statins?
Only once before starting the statin, and then only if you develop symptoms like fatigue, nausea, dark urine, or yellow eyes. Routine testing every 6 months is no longer recommended by the FDA, the American College of Cardiology, or the European Society of Cardiology. Unnecessary testing causes anxiety and leads to more people stopping statins-putting their heart at risk.
Can grapefruit juice affect statin liver safety?
Yes, but only with certain statins. Grapefruit juice blocks an enzyme (CYP3A4) that breaks down atorvastatin, simvastatin, and lovastatin. This can increase blood levels of these statins, raising the risk of side effects-including liver enzyme spikes. If you take one of these, avoid grapefruit juice. Rosuvastatin, pravastatin, and fluvastatin are not affected.
Is coenzyme Q10 worth taking with statins?
It may help reduce mild liver enzyme elevations. In one trial, 100mg daily cut ALT spikes by 43%. But there’s no proof it prevents heart attacks or improves long-term outcomes. It’s not a substitute for the statin. If you’re concerned about liver enzymes, talk to your doctor about switching statins first. CoQ10 is a supplement, not a treatment.
What Comes Next?
If you’ve been told to stop your statin because of liver enzymes, ask for a second opinion. Ask for a repeat test. Ask if other causes have been ruled out. Ask if switching to pravastatin or rosuvastatin is an option.
Don’t let fear of a lab number cost you your heart. Statins save lives. Liver enzyme elevations? Almost always just noise.

Timothy Davis
January 28, 2026 AT 20:12Let’s cut through the noise: elevated liver enzymes on statins are almost always benign. The FDA ditched routine monitoring in 2012 because it was causing more harm than good. People panic, quit their meds, and end up in the ER with MI. The data is crystal clear-less than 1 in 10,000 get serious liver injury. Meanwhile, statins prevent 39 heart events per 1,000 patients over five years. That’s not a risk. That’s a bargain.
And before you blame the statin, check for NAFLD, alcohol, or acetaminophen. I’ve seen 12 patients in the last year with ALT 2x ULN-all had fatty liver or drank 2-3 beers nightly. The statin was just the scapegoat. Stop the panic. Start the logic.
Brittany Fiddes
January 29, 2026 AT 01:21Oh, here we go again-the American medical establishment, pretending it’s ‘evidence-based’ while ignoring the real cost of pharmaceutical propaganda. You’re telling me we should just keep taking a drug that *biologically stresses liver mitochondria* because ‘it’s statistically safe’? Please. The fact that 0.5–2% of people show enzyme elevation means the drug is *interfering with cellular function*. That’s not noise-that’s a biological signal.
And don’t get me started on how the FDA’s guidelines were shaped by industry lobbying. In Britain, we don’t just rubber-stamp every pill that comes with a ‘lifesaving’ label. We ask: What’s the *quality* of life? What’s the *long-term* burden? You’re trading a silent, reversible enzyme spike for a lifetime of chemical dependency. That’s not wisdom. That’s surrender.
Ambrose Curtis
January 29, 2026 AT 06:32Bro, I had the exact same thing happen. Started on 20mg atorvastatin, ALT jumped from 30 to 140. Went full panic mode, almost quit. Then my doc said, ‘Wait, have you been drinking?’ Turns out I’d been having 2 beers after work every night. Cut that out, kept the statin, retested in 5 weeks-back to 32.
Also switched to pravastatin after that just to be safe. No issues since. Two years now. Heart’s good, liver’s good. Don’t overthink it. Rule out alcohol, fatty liver, Tylenol. Then if it’s still up, switch statins. 70% of people bounce back fine. Don’t let fear kill your heart.
PS: Grapefruit juice is a sneaky one. I didn’t even know it messed with statins until my pharmacist called me out.
Linda O'neil
January 30, 2026 AT 11:21This is such an important post-thank you for laying it all out so clearly! So many people are scared to take statins because of a simple blood test result, and it breaks my heart. Your heart is worth protecting. Your liver? It’s resilient. Most of the time, it’s just saying ‘Hey, something else is going on!’
If you’re on a statin and you’re worried, talk to your doctor-but don’t stop without a plan. And if your doc says ‘Stop it,’ ask them: ‘What’s the plan if I keep going?’
You’re not weak for taking a pill that keeps you alive. You’re smart. And you’re not alone. I’ve helped 15 patients stay on their statins through enzyme spikes. Every single one is still here, healthy, and alive. You got this.
Robert Cardoso
February 1, 2026 AT 08:40The entire premise is flawed. You’re treating a statistical artifact as a clinical endpoint. ALT and AST are not biomarkers of liver health-they’re markers of hepatocyte membrane permeability under stress. The fact that statins cause mild, transient increases doesn’t mean they’re safe. It means they’re *biochemically disruptive*. The absence of liver failure doesn’t equal absence of subclinical damage.
And yet, the medical community has turned this into a dogma: ‘Don’t stop the statin.’ Why? Because the alternative is admitting that we prescribe drugs with unknown long-term cellular consequences for asymptomatic conditions. The real risk isn’t the statin-it’s the institutional inertia that refuses to question it.
CoQ10? A placebo bandaid. The real solution is lifestyle. Diet. Exercise. Not more pills to fix the side effects of other pills.
James Dwyer
February 2, 2026 AT 15:57I’ve been on statins for 12 years. My liver enzymes went up once-just a little. I didn’t stop. I didn’t panic. I just waited, retested, and kept going. I’m still here. My cholesterol’s under control. My heart’s fine.
Don’t let a lab number scare you into giving up the thing that’s keeping you alive. Your future self will thank you.
Jeffrey Carroll
February 4, 2026 AT 09:33While the data presented is compelling and largely accurate, the tone of this post risks minimizing legitimate patient concerns. The biochemical mechanism of statin-induced enzyme elevation-mitochondrial stress via lipophilic penetration-is not trivial. Even if the incidence of clinical hepatotoxicity is low, the psychological burden of elevated enzymes is real and often unaddressed.
Furthermore, the suggestion that patients should ‘push back’ against routine testing may inadvertently discourage vigilance in high-risk populations, such as the elderly or those on polypharmacy. A nuanced approach is required: not blanket dismissal, but informed, individualized monitoring.
For many, the fear of liver damage is not irrational-it is the product of decades of medical messaging that equates abnormal labs with disease. That messaging must be corrected, but not by replacing fear with dogma.
doug b
February 4, 2026 AT 22:40Simple truth: if your enzymes are up but you feel fine, keep taking your statin. If you feel like crap-jaundice, dark pee, tired all the time-then stop and call your doc.
Most people who quit statins over a little liver spike end up in the hospital with a heart attack. That’s not a myth. That’s data.
Switch to pravastatin if you’re worried. Cut the booze. Stop the Tylenol. Get tested for hepatitis. Do the easy stuff first.
Don’t let a number ruin your life. Your heart’s counting on you.
SRI GUNTORO
February 6, 2026 AT 16:14It is not the statin that is the problem-it is the modern world’s obsession with quick fixes. You take a pill to fix cholesterol, then another pill to fix the side effect, then another to fix the side effect of that pill. Where is the discipline? Where is the diet? Where is the fasting? Where is the prayer?
Our bodies were not made for synthetic chemicals. We have forgotten how to heal ourselves. The liver enzyme rise is a divine signal: slow down. Eat real food. Move. Rest. Stop relying on pills to do the work of your soul.
God does not bless those who poison their temples with chemical compromises. Heal naturally. Or suffer the consequences.