When your hand starts shaking for no reason-especially when you're sitting still-it’s easy to brush it off as nerves or fatigue. But if that tremor won’t go away, and your muscles feel stiff like they’re wrapped in rubber bands, it might be something deeper. For over 10 million people worldwide, this isn’t just a passing phase. It’s Parkinson’s disease.
What’s Really Happening in the Brain?
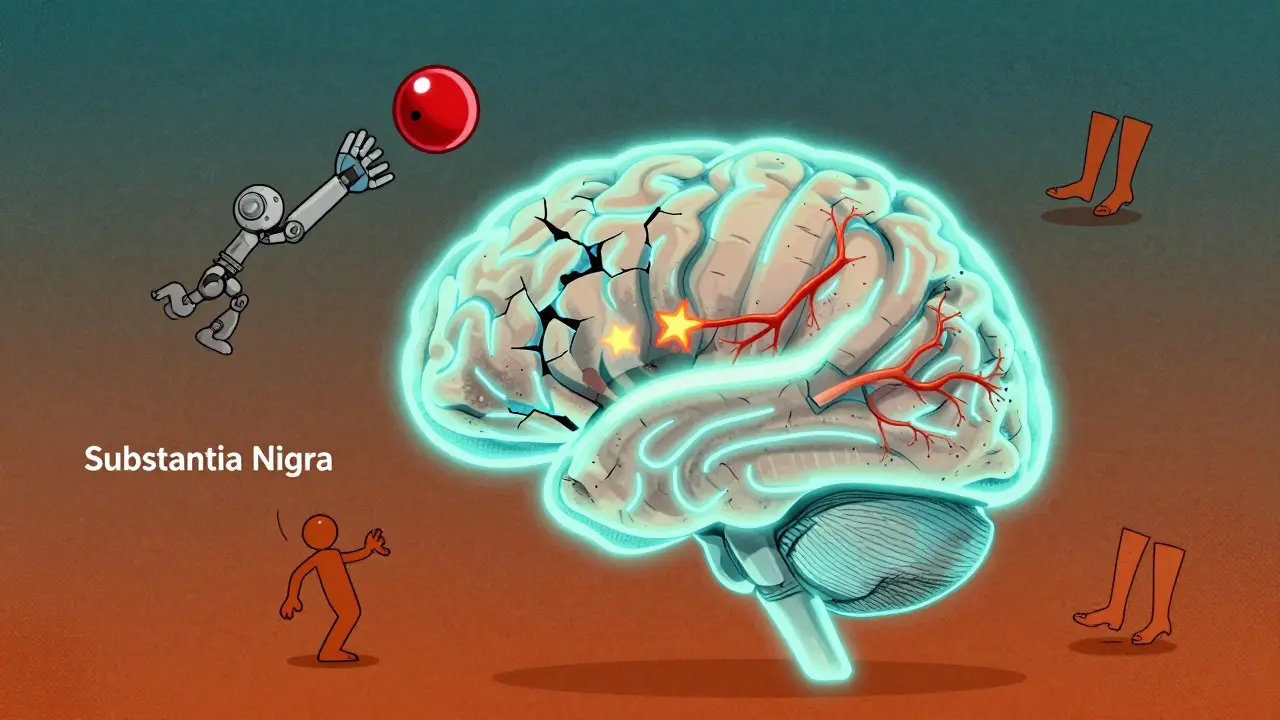
Parkinson’s isn’t just about shaking hands. At its core, it’s a breakdown in the brain’s ability to control movement. A small group of nerve cells in the substantia nigra, a region deep in the brain, slowly die off. These cells make dopamine, a chemical messenger that tells your muscles when and how to move. By the time symptoms show up, you’ve already lost 60 to 80% of those dopamine-producing cells. That’s not a small loss-it’s like trying to drive a car with most of its engine missing. The result? Your movements get slower, stiffer, and less precise. You might notice you don’t swing your arms when you walk. Your handwriting gets smaller. Buttoning a shirt becomes a chore. These aren’t just inconveniences. They chip away at independence.The Three Big Motor Symptoms
There are four main motor symptoms of Parkinson’s, but three stand out early on: tremor, stiffness, and slowness. Let’s break them down.Tremor is what most people think of first. It’s not the kind of shake you get from caffeine. It’s a resting tremor-happening when your hand is relaxed, like when you’re sitting with your arms in your lap. Often, it starts in just one hand, usually the dominant one. The classic sign? A pill-rolling tremor, where your thumb and forefinger rub together like you’re rolling a tiny pill. It fades when you move your hand or fall asleep. Stress, fatigue, or strong emotions can make it worse. About 80% of people with Parkinson’s get this tremor at some point.
Stiffness (or rigidity) is harder to ignore. It’s not just sore muscles. It’s your muscles resisting movement, even when someone else tries to move your arm for you. Doctors describe it as either cogwheel (jerky, like turning a rusty gear) or lead-pipe (smooth, constant resistance). This stiffness doesn’t just make you feel tight-it can cause painful cramps, especially in the legs or neck. About 73% of people report trouble with fine motor tasks like writing or tying shoelaces within the first three years.
Slowness (bradykinesia) is often the most disabling. It’s not laziness. It’s your brain struggling to start and keep up movements. Getting out of a chair takes longer. Walking becomes shuffling. Your face loses expression. You blink less. This symptom shows up early, often before tremor, and it’s the one that most affects daily life.
Why Dopamine Replacement Is the Cornerstone of Treatment
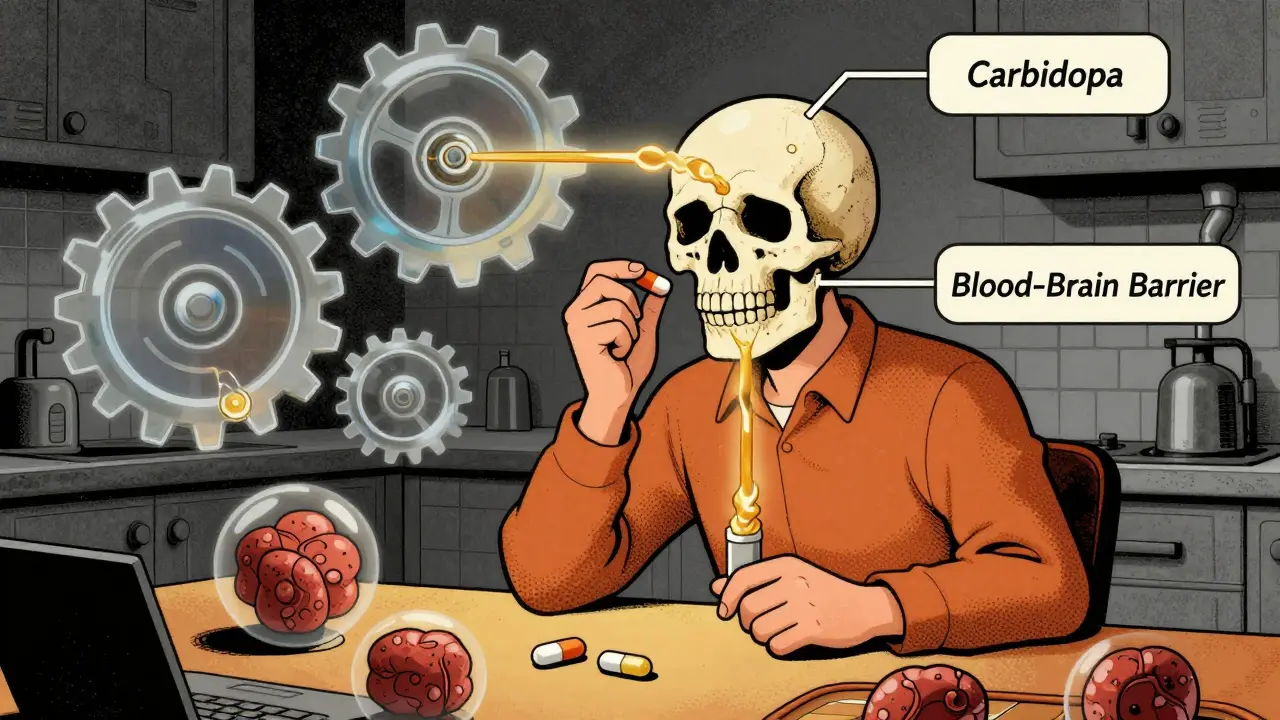
There’s no cure for Parkinson’s. But there’s a treatment that works-really well-at least at first. It’s called dopamine replacement therapy.The brain can’t use dopamine directly because it can’t cross the blood-brain barrier. So instead, doctors give you levodopa-a chemical your brain can turn into dopamine. Levodopa is almost always combined with carbidopa, which stops it from breaking down in your body before it reaches the brain. This combo, sold as Sinemet or in generics, has been the gold standard since the 1970s.
For most people, levodopa is a game-changer. Within 30 to 60 minutes of taking it, movement improves. Walking gets easier. Tremors quiet down. People often describe it as a “rebirth.” Studies show up to 70% improvement in motor symptoms during the first few years-the so-called “honeymoon period.”
But here’s the catch: levodopa doesn’t fix the brain. It doesn’t stop the nerve cells from dying. It just replaces what’s missing. And over time, as more cells die, the body gets less efficient at using the drug.
The Downside of Long-Term Use
After 5 to 10 years, many people start experiencing complications. The biggest ones are:- Wearing-off: The medicine works for only 2-3 hours instead of 4-6. You feel fine, then suddenly, you’re stuck again-like a battery running out.
- On-off fluctuations: You swing unpredictably between being able to move and being frozen, sometimes multiple times a day.
- Dyskinesias: Involuntary, dance-like movements. They’re not painful, but they’re embarrassing and exhausting. Up to 40-50% of people on long-term levodopa get them.
One patient on a Parkinson’s support forum wrote: “After eight years, my ‘on’ time dropped from six hours to two. I’m shaking again, but now I’m also flailing my arms like I’m conducting an orchestra.”
That’s why doctors now take a different approach. Instead of starting levodopa right away, especially in younger patients, they often begin with dopamine agonists-drugs like pramipexole or ropinirole. These mimic dopamine directly in the brain. They’re about 30-50% as effective as levodopa, but they cause fewer dyskinesias early on. Many people stay on them for years with good control.
But here’s the truth: most people eventually need levodopa. About 60% of patients end up on a combination of both. The goal isn’t to avoid levodopa forever-it’s to delay its side effects until they’re absolutely necessary.
Timing, Food, and the Hidden Challenges
Taking dopamine meds isn’t as simple as popping a pill. Timing matters. Protein-especially from meat, dairy, or eggs-can block levodopa from being absorbed. That’s why many patients are told to take their medication 30 minutes before meals or an hour after. Some even switch to low-protein diets during the day.Another issue? Cost. Generic levodopa/carbidopa costs about $600 a year. But extended-release versions like Rytary? Around $5,800. And if you’re having sudden “off” episodes, there’s Inbrija-an inhaled form of levodopa. It works in 10 minutes but runs $3,700 a month.
Managing all this is a full-time job. On average, people spend 15 minutes a day on meds early on. By mid-stage, that jumps to 45 minutes. Nearly 80% need help from a caregiver to keep track of doses, meals, and timing. And here’s a sobering stat: only 35% of community neurologists follow all the recommended guidelines for dosing and timing.

What’s Next? Beyond Pills
Research is moving fast. One promising option is a continuous dopamine infusion under the skin-like a tiny pump that delivers medicine all day. A 2022 trial showed it added 2.5 more “on” hours per day compared to oral meds. Another is gene therapy, trying to get the brain to make its own dopamine again. Still experimental, but hopeful.And then there’s personalized medicine. Scientists are looking at your genes-specifically, how your body breaks down dopamine (via COMT and MAO-B enzymes). Some people metabolize levodopa fast. Others slow. That could one day tell your doctor exactly which drug and dose you need, before you even start.
For now, the best strategy remains simple: start low, go slow. Use the lowest effective dose. Monitor closely. Combine meds wisely. And don’t ignore non-drug help-physical therapy, exercise, speech therapy. Movement is medicine, too.
It’s Not Just About the Brain
Parkinson’s affects more than movement. Depression, sleep problems, constipation, and loss of smell often come before tremor. These are part of the disease, too. But they’re rarely talked about. Treating the tremor won’t fix the fatigue. Fixing the stiffness won’t help the anxiety. That’s why holistic care matters.The disease is expected to double in number by 2040. That means more families will face these choices: when to start levodopa, how to handle side effects, how to keep living well. There’s no perfect answer. But knowing the science behind the shaking, the stiffness, and the pills can help you make smarter, calmer decisions.
There’s no cure yet. But with the right approach, many people live full, active lives for decades. It’s not about stopping the disease. It’s about managing it-on your terms.

Juan Reibelo
January 24, 2026 AT 03:29That pill-rolling tremor description? Chillingly accurate. I’ve seen it in my dad-his fingers just… rotate, like he’s grinding something invisible. And the stiffness? Like trying to move a statue that forgot it was supposed to bend. It’s not laziness. It’s biology betraying you. I wish more people understood that.
Amelia Williams
January 24, 2026 AT 09:27I love how you broke this down-it’s like a textbook made by someone who actually lives with this. The dopamine replacement analogy? Perfect. Carbidopa is the bouncer keeping levodopa from getting wasted at the club. And yes, the ‘honeymoon period’? Real. Then it hits you-suddenly, you’re a human battery with a glitchy charger. But hey, movement is medicine. I walk 5 miles every morning. Still shaky. Still alive. Still winning.
Viola Li
January 25, 2026 AT 04:12Everyone’s acting like levodopa is some miracle cure. It’s not. It’s a bandaid on a bullet wound. And now we’re all pretending it’s the only option? What about stem cells? What about gene editing? We’ve had CRISPR for years. Why are we still dosing people with 1970s chemistry while billionaires fund Mars colonies? This isn’t science-it’s complacency.
venkatesh karumanchi
January 26, 2026 AT 12:10My uncle had Parkinson’s. He never took levodopa. Said he didn’t want to feel like a machine. He did yoga, sang every morning, ate turmeric like candy. Lived 14 years after diagnosis. No dyskinesias. No ‘off’ times. Just… peace. Maybe the answer isn’t always in the pill bottle.
Jenna Allison
January 27, 2026 AT 12:33Important note: COMT inhibitors like entacapone extend levodopa’s half-life by blocking its peripheral metabolism. MAO-B inhibitors like selegiline reduce dopamine breakdown in the CNS. Both are adjuncts-not alternatives. And yes, protein competition at the BBB is real. Timing matters because L-DOPA competes with large neutral amino acids for LAT1 transporters. If you’re on it, space meals. Or switch to protein redistribution diets. This isn’t opinion-it’s pharmacokinetics.
Kat Peterson
January 28, 2026 AT 11:51OMG I CRIED reading this 😭😭😭 Like… I just got diagnosed last month and I thought I was losing my mind. But now I get it. The tremor wasn’t anxiety. The stiffness wasn’t ‘getting old.’ I’m not broken. I’m just… rewired. And I’m not alone. Thank you for writing this like a letter to your best friend. 💕❤️🫂
Shanta Blank
January 29, 2026 AT 03:39Let’s be real-levodopa is the opioid of neurology. We’re addicted to it because it works, but we’re ignoring the wreckage. Dyskinesias? They’re not side effects-they’re the price of survival. And who pays? The patient. The caregiver. The family. We’re not treating Parkinson’s. We’re just delaying the inevitable with a chemical tourniquet. And now we’re charging $3,700 a month for an inhaler? That’s not healthcare. That’s extortion dressed in white coats.
Tiffany Wagner
January 30, 2026 AT 11:23My mom’s on Rytary now. She takes it before breakfast. No meat. No eggs. Just oatmeal and tea. It’s a whole routine. I help her set alarms. She forgets sometimes. But when it works? She dances in the kitchen. Just a little. But it’s enough. I’m glad someone finally said it-movement is medicine. We walk every day. Even if it’s slow. Even if it’s shaky. We still go.
Kevin Waters
January 30, 2026 AT 15:10Thanks for the clarity. I’ve been telling my cousin for months to talk to a movement disorder specialist, not just his GP. The guidelines exist for a reason. And yes, physical therapy isn’t optional-it’s essential. I’ve seen people regain balance, speech, even handwriting with consistent PT. It’s not magic. But it’s powerful. And it’s free. Or covered by insurance. Stop waiting for a pill. Start moving.