Antihistamine Cross-Reactivity Checker
If you've had a paradoxical reaction to an antihistamine, this tool helps identify which other antihistamines you may also react to. This is based on scientific research about receptor-level malfunctions, not IgE-mediated allergies.
Next Steps
- Stop taking all antihistamines immediately
- Consult a specialist allergist who understands paradoxical reactions
- Bring a detailed list of all antihistamines you've taken
- Ask about supervised oral challenges for confirmation
- Check for underlying infections that may be contributing
It’s one of the most common mistakes people make with allergies: reaching for an antihistamine when symptoms flare up. You expect relief. Instead, your skin breaks out in hives. Your face swells. Your throat tightens. You didn’t get better-you got worse. And it’s not just in your head. This isn’t rare. It’s real. And it’s called antihistamine allergy.
When the Cure Makes It Worse
Antihistamines are supposed to block histamine, the chemical your body releases during an allergic reaction. They’re the go-to for sneezing, itchy eyes, and hives. But for a small number of people, these drugs don’t block histamine-they trigger it. Instead of calming the immune system, they accidentally turn on the very receptors they’re meant to shut down. This is called a paradoxical reaction. It’s not an allergy to the pill’s filler or dye. It’s your body misreading the drug as histamine itself. A 2017 study in Allergol Select followed a woman who developed chronic hives from every major antihistamine she took-including loratadine, cetirizine, and fexofenadine. She’d taken them for years, thinking they were helping. Then she stopped. The hives vanished. The twist? She had an underlying infection. Once that was treated, she stayed symptom-free. But the key takeaway: the antihistamines themselves were the problem.How Does This Even Happen?
Your body has H1 receptors-tiny locks on cells that histamine turns on. Antihistamines are supposed to fit into those locks and keep them shut. But in some people, the shape of their receptors is slightly different. A 2024 study in Nature Communications used cryo-electron microscopy to see exactly how antihistamines bind to these receptors. They found that in most people, the drug locks the receptor in the “off” position. But in those with rare receptor variations, the same drug can lock it in the “on” position. It’s like turning a key the wrong way. The lock clicks open instead of closed. This isn’t about allergies to ingredients like lactose or dyes. It’s about your genetics. Some people have H1 receptor polymorphisms-tiny genetic differences-that change how the drug behaves. These changes are invisible on standard allergy tests. That’s why so many people are misdiagnosed. They’re told their hives are “chronic idiopathic urticaria,” when the real trigger is the medicine they’re taking to treat it.Which Antihistamines Cause This?
It’s not just one type. Both first- and second-generation antihistamines have been linked to paradoxical reactions. First-generation drugs like diphenhydramine (Benadryl) and pheniramine are older. They cross into your brain, which is why they make you sleepy. But they’re also more likely to interact with other receptors, like muscarinic ones. That adds another layer of risk. Second-generation drugs-loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra), desloratadine (Clarinex), and levocetirizine (Xyzal)-are marketed as non-drowsy. But they’re not safer when it comes to paradoxical reactions. In fact, the 2017 study showed reactions to all of them. Even piperidine-based drugs like ebastine and mizolastine, and piperazine-based ones like hydroxyzine, triggered hives in the same patient. The takeaway? No antihistamine is completely safe for everyone. If you’ve ever had a reaction after taking one, don’t assume it’s just a coincidence.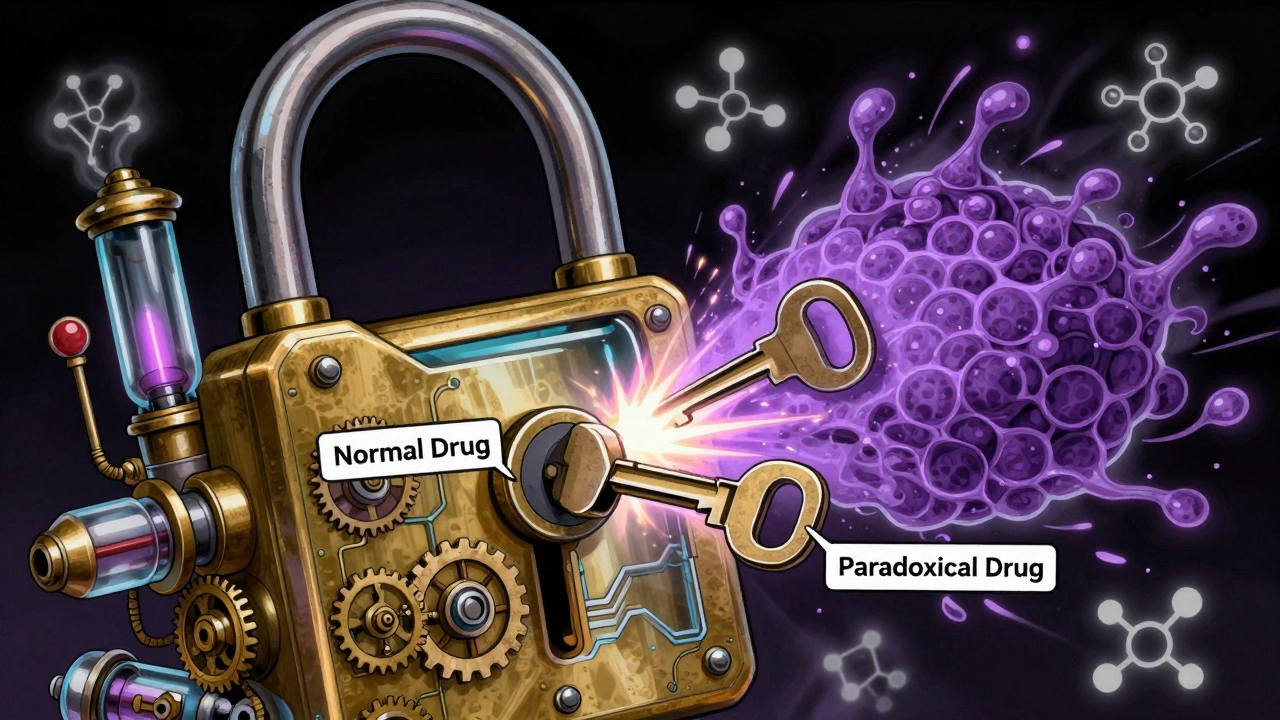
Cross-Reactivity: The Hidden Trap
Here’s the scary part: if you react to one antihistamine, you might react to others-even if they’re from different chemical families. A 2018 case in the Korean Journal of Pediatrics showed a child who broke out in hives after taking ketotifen, even though skin tests for ketotifen came back negative. The child had already reacted to cetirizine and loratadine. The reaction didn’t happen right away-it took 120 minutes. And it got worse with higher doses. That’s not an allergic reaction you can test for with a simple prick. That’s a delayed, dose-dependent, systemic response. Doctors used to think cross-reactivity only happened within the same chemical group-like all piperazines reacting together. But now we know that’s wrong. Reactions can jump between classes. One person might react to cetirizine and fexofenadine, even though they’re chemically unrelated. Another might react to diphenhydramine and hydroxyzine, even though one is sedating and the other isn’t. The only reliable way to test for this? An oral challenge. But that’s risky. You need a doctor watching you, ready to treat anaphylaxis. And even then, it’s not foolproof. Negative skin tests mean nothing. The only thing that matters is what happens when you swallow the pill.Why Standard Tests Fail
Skin prick tests and blood tests for IgE antibodies are great for peanut allergies or pollen. But they’re useless here. Why? Because this isn’t an IgE-mediated allergy. It’s a receptor-level malfunction. Your immune system isn’t producing antibodies. Your H1 receptors are just misfiring. That’s why so many people get misdiagnosed. They’re told they have chronic urticaria. They’re prescribed more antihistamines. Their symptoms get worse. They go from one doctor to another. It takes years. One patient in the 2017 study spent over a year being treated for chronic hives-until someone finally asked, “Have you tried stopping the antihistamines?”What to Do If You Suspect a Reaction
If you’ve taken an antihistamine and your symptoms got worse, here’s what to do:- Stop taking all antihistamines immediately. Even if they’re “non-drowsy” or “prescription-only.”
- Write down every antihistamine you’ve taken in the last 6 months-over-the-counter and prescription.
- Look for patterns. Did your rash start after starting a new pill? Did it get worse when you increased the dose?
- See an allergist who understands paradoxical reactions. Not all do. Ask if they’ve seen cases like this before.
- Ask about oral challenges under supervision. Don’t test yourself at home.
- Check for underlying infections. Chronic sinus infections, H. pylori, or even dental abscesses can trigger or worsen these reactions.
What Can You Take Instead?
If you can’t use antihistamines, you still have options. The goal is to calm the immune response without triggering H1 receptors.- Leukotriene inhibitors like montelukast (Singulair) can help with hives and allergic inflammation. They work on a different pathway.
- Immunosuppressants like cyclosporine are used in severe chronic urticaria when antihistamines fail.
- Omalizumab (Xolair) is an injectable biologic approved for chronic hives. It targets IgE directly, bypassing H1 receptors entirely.
- Corticosteroids (short-term) can break severe flare-ups, but they’re not for daily use.
- Non-drug approaches like cold compresses, avoiding heat and tight clothing, and stress reduction can reduce flare-ups.
The Bigger Picture
Antihistamines are among the most widely used drugs in the world. Millions take them daily. But we treat them like harmless pills. We don’t think about how they interact with your unique biology. The truth? Your body isn’t a one-size-fits-all machine. What works for 99% of people can be dangerous for the other 1%. New research is changing how we design these drugs. The 2024 cryo-EM study revealed a second binding site on the H1 receptor. That means future antihistamines could be built to avoid triggering paradoxical reactions entirely. But until then, awareness is your best defense. If you’ve been told your hives are “unexplained,” and nothing seems to help-ask yourself: What if the medicine is the problem?Frequently Asked Questions
Can you be allergic to antihistamines even if you’ve taken them before without problems?
Yes. Paradoxical reactions can develop over time. Your body’s receptors can change due to genetics, chronic inflammation, or infections. Someone might take cetirizine for years with no issue, then suddenly start breaking out in hives after a viral illness or prolonged stress. It’s not about the dose-it’s about your body’s current state.
Are second-generation antihistamines safer than first-generation ones?
In terms of drowsiness and side effects, yes. But when it comes to paradoxical reactions, no. Studies show reactions happen with both types. Fexofenadine, loratadine, and cetirizine-all second-gen-have all been linked to triggering hives in sensitive individuals. The difference is that second-gen drugs don’t cross the blood-brain barrier, so you won’t feel sedated. But your skin can still react.
If a skin test for an antihistamine is negative, is it safe to take?
No. Skin tests are unreliable for detecting paradoxical antihistamine reactions. A 2018 case showed a patient with negative skin tests for ketotifen still developed severe hives after taking it orally. The only reliable test is an oral challenge under medical supervision. Don’t rely on skin tests alone.
Can antihistamine allergies be cured?
There’s no cure for the receptor sensitivity itself. But many people find relief by avoiding all antihistamines and treating underlying triggers like infections, autoimmune conditions, or chronic stress. Once those are managed, symptoms often improve significantly-even without medication. Some people never need antihistamines again.
What should I do if I react to every antihistamine?
You need a specialist. Ask for a referral to an allergist or immunologist who specializes in chronic urticaria and drug hypersensitivity. Bring a full list of every antihistamine you’ve tried and when you reacted. You may need biologics like omalizumab or immunosuppressants. Don’t keep trying different antihistamines-it could make things worse.

brenda olvera
December 7, 2025 AT 06:49My grandma in Mexico used to say if a pill makes you worse you’re not sick-you’re listening. Stop taking everything and let your body breathe. I did. Hives vanished in three days. No doctor needed.
Love this post.
Thank you.
Akash Takyar
December 8, 2025 AT 11:39While the phenomenon described is indeed rare, it is not without precedent in pharmacogenomics. The H1 receptor polymorphism hypothesis, supported by recent cryo-EM data, suggests a highly individualized pharmacodynamic response. This underscores the necessity for personalized medicine approaches in allergic conditions, rather than population-based prescribing. One must consider not merely the drug’s mechanism, but the structural integrity of the target receptor in the individual.
Thank you for highlighting this critical, under-discussed topic.
Arjun Deva
December 10, 2025 AT 05:48Of course this is happening-Big Pharma doesn’t want you to know antihistamines can make you sicker. They’ve been hiding this since the 90s. Why do you think they pushed second-gen drugs so hard? To make more money while keeping you hooked. And now they’re calling it a ‘paradoxical reaction’ like it’s some mystical glitch. It’s not. It’s a cover-up. The FDA knew. The WHO knew. They just didn’t tell you. You’re being dosed with poison and told it’s medicine.
Wake up.
They’re watching your searches.
Inna Borovik
December 10, 2025 AT 12:33Let’s be real: this is just a fancy way of saying ‘some people are just allergic to everything.’
Meanwhile, 99% of the population uses antihistamines without issue. The fact that you’re making a whole article out of this suggests you’re either over-medicalizing normal variation or you’re fishing for clicks. Either way, this reads like a clickbait trap wrapped in pseudoscientific jargon.
Also, ‘paradoxical reaction’? That’s not a diagnosis. That’s a cop-out term for ‘we don’t know why this happened.’
Stop giving people permission to blame their symptoms on pills they’ve taken for years.
Jackie Petersen
December 10, 2025 AT 14:46America’s medical system is broken. You take a pill, you get worse, you go to a doctor, they give you another pill. Meanwhile, in India, they just drink turmeric milk and sleep it off. Why are we so dependent on chemicals? Why do we think every problem needs a synthetic solution? This isn’t science-it’s corporate laziness. We’re turning people into lab rats for Big Pharma’s profit. And now you’re writing a whole article about it like it’s news? It’s been happening for decades. Wake up, people.
Annie Gardiner
December 11, 2025 AT 08:52What if the real problem isn’t the antihistamine… but the fact that we’ve turned our bodies into battlefields? We’re so obsessed with suppressing symptoms that we’ve forgotten how to listen to them. Maybe your hives aren’t caused by the drug-maybe they’re screaming that your gut is dead, your stress is nuclear, and your immune system is begging for silence. What if the cure was never in the pill… but in the pause?
Just saying.
Rashmi Gupta
December 13, 2025 AT 00:31Interesting. But let’s not pretend this is new. In Ayurveda, we call this ‘ama’-toxic buildup that turns medicine into poison. The body doesn’t react to the drug. It reacts to the imbalance. Antihistamines are like putting a bandage on a broken leg and calling it healing. The real question isn’t ‘which antihistamine?’-it’s ‘why is your system so fragile?’
Also, I tried cetirizine once. Broke out in hives. Stopped. Ate ginger, garlic, neem. Gone in 48 hours. No doctor. No test. Just wisdom.
Andrew Frazier
December 14, 2025 AT 01:22Y’all act like this is some deep mystery. Nah. It’s just science being science. Some people’s receptors are glitchy. Like a bad keyboard key. You don’t blame the keyboard-you just don’t use it. Same here. If you react to antihistamines? Don’t take em. Simple. No need for 10 paragraphs. Also, why are we trusting studies from journals nobody reads? I mean… Nature Communications? That’s like trusting a TikTok influencer with a lab coat.
Kumar Shubhranshu
December 14, 2025 AT 09:45Stop. Listen. If you react to antihistamines, stop taking them. That’s it. No tests. No theories. No articles. Just stop. Your body told you. You ignored it. Now you’re reading this. Do the thing. Simple. Done.
Mayur Panchamia
December 15, 2025 AT 03:14Oh, so now we’re blaming the pills? The system? The corporations? The ‘receptor polymorphisms’? Pfft. I’ve been taking Zyrtec since 2012. Never had a problem. Meanwhile, my cousin in Delhi got hives from eating mangoes. Should we ban mangoes? No. We fix the damn body. You’re not fragile. You’re just lazy. Stop looking for excuses. Get your gut checked. Sleep better. Stop stress-eating. And for god’s sake, stop blaming Big Pharma for your inability to live like a normal human being.
Karen Mitchell
December 16, 2025 AT 20:09It is deeply concerning that such a medically significant phenomenon is being presented as an emerging revelation, when in fact, it has been documented in peer-reviewed literature since the early 2000s. The fact that this requires a viral post to gain attention speaks volumes about the erosion of clinical literacy among the general public. One must question the ethics of publishing such content without emphasizing the extreme rarity of the condition. This risks inducing unnecessary fear, and worse-noncompliance with essential medications among those who genuinely benefit from antihistamines.
Nava Jothy
December 16, 2025 AT 22:43OMG I’ve been this person 😭
Took Zyrtec for 7 years. Hives every time. Thought I was ‘just sensitive.’ Went to 3 allergists. All said ‘it’s chronic urticaria.’ Then I stopped. 3 days later-gone. No meds. No magic. Just… stopped.
Now I use cold showers and aloe. And I cry every time I see someone on Reddit saying ‘try Xyzal’ like it’s a cure.
Thank you for writing this. I finally feel seen.
🫂
Myles White
December 17, 2025 AT 12:20This is actually one of the most compelling pieces I’ve read in a long time. I’ve spent years working in clinical research on drug-receptor interactions, and the idea that a drug can bind to the same receptor and produce diametrically opposed effects based on subtle structural differences is not just fascinating-it’s paradigm-shifting. The 2024 cryo-EM paper was a game-changer because it finally gave us a structural basis for what was previously considered anecdotal. What’s even more profound is the implication for drug design: if we can map the secondary binding site, we might engineer antihistamines that avoid triggering the ‘on’ conformation entirely. This isn’t just about allergies-it’s about rethinking how we design all receptor-targeting drugs. I hope this gets more attention in pharmacology curricula.
olive ashley
December 19, 2025 AT 04:56So let me get this straight. You’re telling me that the one thing I’ve been taking to stop my hives… is the thing causing my hives?
And I’ve been taking it for 11 years.
And every doctor I saw just kept giving me more?
And now you’re telling me skin tests are useless?
And the only way to know is to take it again… and risk anaphylaxis?
So what you’re saying is… I’ve been poisoned by the cure.
And nobody told me.
And I’m supposed to just… stop?
And hope I don’t die?
And pay for a specialist who might not even believe me?
…
Thanks for the reassurance.
Now I feel even worse.
Katie O'Connell
December 20, 2025 AT 02:27While the author presents an intriguing clinical observation, the framing of this phenomenon as a widespread, under-recognized public health crisis is profoundly misleading. The prevalence of paradoxical antihistamine reactions is statistically negligible-estimated at less than 0.01% of users. To elevate this to the level of a universal cautionary tale risks inducing iatrogenic anxiety in millions of patients who derive significant benefit from these medications. The suggestion that standard allergy testing is ‘useless’ in this context is not only inaccurate but dangerous; IgE-mediated reactions do occur, and they are diagnosable. The conflation of receptor-level pharmacodynamic variation with classical immunological allergy is a category error. One must exercise extreme caution in disseminating such information without appropriate nuance and context. This is not enlightenment-it is pharmacological sensationalism.