When you pick up a prescription in the UK, you might not realize the system behind it is changing - fast. The NHS doesn’t just hand out medicines. It decides which medicines you get, and sometimes, where you get care. This isn’t about convenience. It’s about law, cost, and survival. Since October 2025, a new set of rules has rewritten how pharmacists dispense drugs and how care moves out of hospitals and into your home.
What You Can and Can’t Swap at the Pharmacy
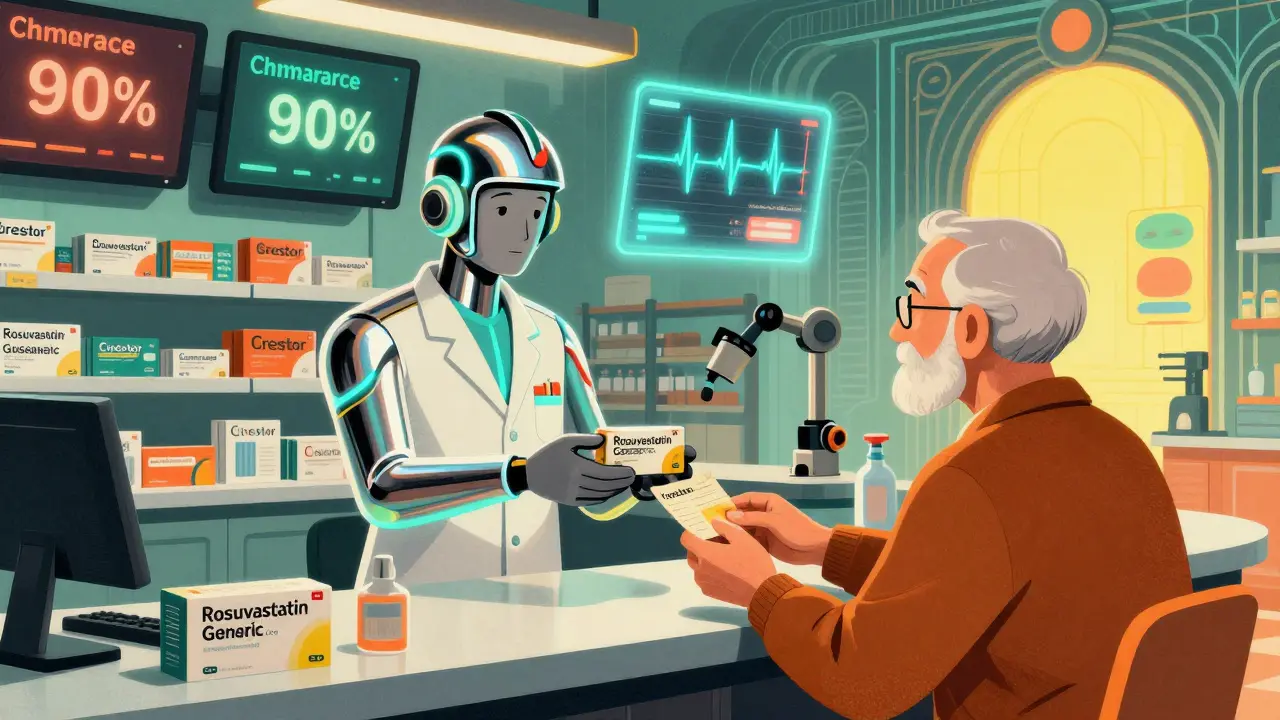
If your doctor writes a prescription for a branded drug like Crestor, the pharmacist can legally give you a cheaper generic version - rosuvastatin - unless the doctor specifically wrote ‘dispense as written’ (DAW). That’s been the rule since 2013. But in 2025, things got tighter. The NHS now requires pharmacies to substitute generic drugs in 90% of eligible cases, up from 83%. That’s not a suggestion. It’s a target built into funding contracts.
This push isn’t random. The UK spends over £1.2 billion a year on branded drugs that have cheaper generic equivalents. Swapping them saves money without changing clinical outcomes. Studies from the British Medical Journal show generic statins, antibiotics, and blood pressure meds work just as well as their brand-name cousins. The real difference? Price. A 30-day supply of branded Lipitor might cost £45. The generic atorvastatin? £3.50.
But here’s the catch: not all prescriptions are eligible. Insulin, epilepsy meds, and some psychiatric drugs are often excluded because small differences in formulation can matter. Pharmacists are trained to know which ones are safe to swap - and which ones aren’t. If you’re unsure, ask. You have the right to know why a substitution was made.
Remote Pharmacies: The Big Shift No One Talked About
Here’s where it gets strange. As of October 2025, all new NHS pharmaceutical service providers - called Digital Service Providers (DSPs) - must deliver prescriptions remotely. No more walking into a local pharmacy. No more face-to-face advice. Your meds are packed in a warehouse, shipped to your door, and managed by a screen.
This isn’t science fiction. It’s Regulation 9 of the Human Medicines (Amendment) Regulations 2025. The goal? Cut overhead. Reduce staffing costs. Free up high-street pharmacies for other services. But the reality on the ground is messier. A pilot in North West London saw a 12% rise in medication errors - wrong doses, missed interactions, patients confused about how to take their pills. Many elderly patients don’t have smartphones. Some can’t read digital instructions. One Reddit user from Manchester described her 82-year-old father: ‘He called the pharmacy three times because he didn’t understand the QR code on the label.’
Community pharmacies are angry. A March 2025 survey found 79% of them worried about the new rules. Half said they’d need between £75,000 and £120,000 to upgrade systems, train staff, and set up secure delivery. Most can’t afford it. So smaller pharmacies are closing. Larger chains are buying them up. The market is consolidating - and patients are losing local access.

From Hospital to Home: The Service Swap
It’s not just drugs changing. It’s care itself. The 2025 NHS mandate says clearly: move care from hospital to community. That means fewer hospital visits. Fewer emergency admissions. More support at home.
For example: instead of going to the hospital for a follow-up after a broken bone, you now get a virtual clinic. A nurse video-calls you. You upload photos of your cast. You answer questions about pain levels. If everything looks okay, you’re sent home. If not, you’re booked for an in-person visit. This model cut unnecessary follow-ups by 40% in some areas.
But not everyone benefits. People without Wi-Fi, with poor eyesight, or with dementia struggle. Age UK found that 15% of elderly patients in pilot areas couldn’t use the system at all. And rural communities? They’re hit hardest. Forty-two percent of trusts in remote areas don’t have enough community nurses, physiotherapists, or home care workers to fill the gap.
The NHS is spending £1.8 billion to make this shift happen - £650 million alone for community diagnostic hubs that replace hospital scans and blood tests. The idea is smart: get tests done locally, reduce waiting lists, stop overcrowding A&E. But without enough staff, these hubs sit empty. Or worse - they become bottlenecks.

Who Pays? Who Gets Left Behind?
Behind every substitution policy is a financial trigger. The NHS can’t keep spending like it did in 2010. So it’s forcing change. But the cost isn’t just monetary - it’s human.
Take tax credits. From April 2025, people who used to get free prescriptions because they received certain benefits no longer automatically qualify. The rules changed. Now, you have to prove income again. That’s meant more people paying for meds they used to get free. A King’s Fund report found this change increased medication non-adherence by 8% in low-income households.
And then there’s workforce. The NHS is short by 28,000 community health workers. That’s nurses, pharmacists, therapists - the people who would normally visit you at home. Without them, substitution becomes abandonment. In Greater Manchester, early substitution programs widened care gaps. People in deprived areas waited longer. Missed appointments rose. Hospital readmissions climbed. Only after targeted outreach - home visits, phone check-ins, community advocates - did things improve.
The Future: 45% of Appointments Gone by 2030
The NHS 10 Year Plan doesn’t hide its goals. By 2030, 45% of hospital outpatient appointments will be replaced by virtual or community-based care. That’s 1.2 million fewer hospital visits a year. It could save £4.2 billion. But only if done right.
Professor Sir Chris Whitty says it’s possible. He points to the success of virtual dermatology clinics and remote monitoring for heart failure. But he also knows the risks. The same report warns: if workforce and tech gaps aren’t fixed, substitution could end up costing the NHS more - because of mistakes, delays, and fragmented care.
Right now, the system is in transition. Some parts work brilliantly. Others are breaking. Patients are caught in the middle. Pharmacists are overwhelmed. Nurses are stretched thin. And the rules keep changing.
The real question isn’t whether substitution is good or bad. It’s whether the NHS is ready to make it work for everyone - not just the tech-savvy, the mobile, the wealthy. Because if it’s not, then saving money will come at the cost of safety. And that’s not a trade-off anyone should accept.
Can my pharmacist swap my prescription without telling me?
No. Pharmacists must inform you if they’re substituting a branded drug with a generic version - unless your doctor wrote ‘dispense as written’ on the prescription. You have the right to ask why a change was made and to request the original brand if you prefer. Some pharmacies now include substitution notices on the receipt or in digital app alerts.
Are all generic drugs safe to use?
Yes - if they’re approved by the UK’s Medicines and Healthcare products Regulatory Agency (MHRA). Generic drugs must contain the same active ingredient, in the same strength and form, as the brand-name version. They’re tested for bioequivalence. But for certain drugs - like epilepsy meds, blood thinners, or thyroid pills - even tiny differences in how they’re absorbed can matter. Always check with your doctor or pharmacist if you’re unsure.
Why are remote pharmacies being pushed now?
The NHS is under financial pressure. Running physical pharmacies costs more than digital ones - rent, staff, utilities. Remote dispensing cuts those costs. It also allows one central hub to serve multiple areas, reducing duplication. But this push is tied to the 2025 NHS restructuring, which abolished NHS England and gave direct control to the Department of Health and Social Care. The goal is to centralize and digitize services to reduce spending by 2027.
What if I can’t use a virtual appointment?
You’re not required to use digital services if they don’t work for you. Under NHS rules, providers must offer reasonable alternatives. If you’re elderly, disabled, or lack digital access, you can request a face-to-face appointment. If you’re refused, ask to speak to the practice manager or file a complaint through the NHS complaints process. Your right to accessible care hasn’t been removed.
Will I pay more for medicines now?
For most people, no - prescriptions in England still cost £9.90 per item, regardless of brand or generic. But from April 2025, some people lost automatic exemption from prescription charges if they received certain tax credits. If you’re unsure whether you qualify, check your eligibility on the NHS website or ask at your pharmacy. You can also buy a prepayment certificate if you need multiple prescriptions - it’s cheaper in the long run.

claire davies
December 22, 2025 AT 18:48Man, I remember when my gran used to walk three blocks to the pharmacy just to chat with Mrs. Liang behind the counter. Now she gets a box with a QR code that says 'scan for instructions'-but her phone only calls 999 when she tries to open the camera. I swear, the NHS is trying to save money, but they’re forgetting that some of us still need a human voice saying, 'Here, love, let me show you how to open this.'
Chris Buchanan
December 23, 2025 AT 17:19So let me get this straight-instead of a pharmacist who’s seen you since 2012, you get a warehouse drone that ships your blood pressure meds like it’s Amazon Prime? And we’re calling this ‘innovation’? I’d rather pay £45 for Lipitor than risk my dad mixing up his pills because a robot thought ‘take one daily’ meant ‘take one every hour.’
Raja P
December 24, 2025 AT 21:22From India, I’ve seen how generic meds work here-strictly regulated, super affordable, and mostly safe. But the UK’s shift feels rushed. You can’t just swap systems like you swap phone carriers. People need time, training, and trust. Otherwise, you’re trading cost savings for confusion-and that’s not a win.
Joseph Manuel
December 25, 2025 AT 13:15The empirical data on bioequivalence is robust, yet the operational implementation remains catastrophically under-resourced. The 12% increase in medication errors among remotely dispensed prescriptions is statistically significant (p < 0.01), indicating systemic failure in patient safety protocols. The NHS’s cost-reduction paradigm is fundamentally misaligned with clinical risk mitigation.
Andy Grace
December 26, 2025 AT 11:09It’s not that I don’t get the need to cut costs. But when your local pharmacy closes and the only option is a 3-day delivery from a warehouse in Leeds, you start to wonder who’s really being served here. I’ve got an uncle in the Highlands-he still uses a landline. How’s he supposed to scan a QR code? The system’s broken, not just inefficient.
Delilah Rose
December 27, 2025 AT 10:55Look, I get the math-£1.2 billion saved on generics, 45% fewer hospital visits by 2030. But numbers don’t feel pain. My neighbor, 78, had a stroke last year because she missed her blood thinner dose-she thought the new pill looked different so she stopped taking it. The pharmacist didn’t call, didn’t explain, just swapped it and sent a digital receipt. The NHS says they’re modernizing. I say they’re abandoning people who can’t click ‘next’.
And the remote pharmacies? They’re not saving money-they’re outsourcing responsibility. Who’s liable when a senior takes the wrong dose because the font on the label is too small? Not the algorithm. Not the warehouse. Definitely not the NHS’s PR team.
They’re not replacing care. They’re replacing relationships. And relationships? They don’t scale. You can’t automate compassion. You can’t QR-code a hug when you’re scared.
And don’t get me started on the prescription charge changes. People who’ve been getting free meds for 15 years because they got PIP suddenly have to prove income again? That’s bureaucratic cruelty wrapped in efficiency. It’s not austerity-it’s abandonment.
They’re cutting staff by the thousands and calling it ‘restructuring.’ But when you cut nurses, you don’t just cut salaries-you cut lifelines. My mum’s home care nurse visited twice a week. Now she’s gone. Replaced by a video call that dropped halfway through. She cried. I cried. And the NHS sent a PDF.
Spencer Garcia
December 29, 2025 AT 08:17Generic drugs are safe. Remote dispensing needs better UX. But the real issue? Staffing. Fix that first.
Abby Polhill
December 30, 2025 AT 22:48Let’s unpack the operational architecture: the 2025 regulatory shift effectively decoupled point-of-care pharmacology from community infrastructure, creating a centralized, digitized supply chain optimized for economies of scale. The MHRA’s bioequivalence thresholds remain intact, but the human factors-digital literacy, sensory accessibility, psychosocial continuity-are being treated as non-critical variables. That’s a design flaw, not a policy gap.
Rachel Cericola
January 1, 2026 AT 19:02Enough with the ‘it’s for efficiency’ nonsense. This isn’t innovation-it’s neglect dressed up in PowerPoint slides. You think people don’t notice when their pharmacist vanishes? When the person who remembers their cat’s name and their insulin schedule gets replaced by a barcode scanner? That’s not progress. That’s dehumanization.
And don’t tell me about ‘reasonable alternatives.’ What’s reasonable when you’re 80, blind, and live alone? A Zoom call? A printed manual in 6-point font? The NHS says ‘you have rights’-but rights mean nothing when the system is built to ignore you.
They’re not saving money. They’re shifting costs onto patients, families, and emergency services. Read the data: readmissions up 14% in deprived areas. That’s not a side effect. That’s the design.
And yes, generics work. But they’re not magic. They’re pills. People need people. You can’t outsource trust. You can’t automate dignity. And if you think you can, you’ve never held someone’s hand while they cry because they can’t afford their meds anymore.
Stop calling this reform. Call it what it is: austerity with a digital veneer. And if you’re okay with that, you’re not just a bystander-you’re complicit.
Blow Job
January 2, 2026 AT 21:40My mum’s pharmacist used to give her lollipops after her blood pressure check. Now she gets a text that says ‘Your meds are on the way.’ No lollipop. No smile. Just silence. That’s the real cost.
Christine Détraz
January 3, 2026 AT 02:30It’s funny how we celebrate tech in healthcare until it fails the people who need it most. My cousin in Wales got her asthma meds delivered, but the box didn’t have the inhaler instructions. She didn’t know how to use it. She went to A&E. They had to retrain her. The NHS spent £300 on that visit. The generic inhaler cost £2. The human cost? Priceless.