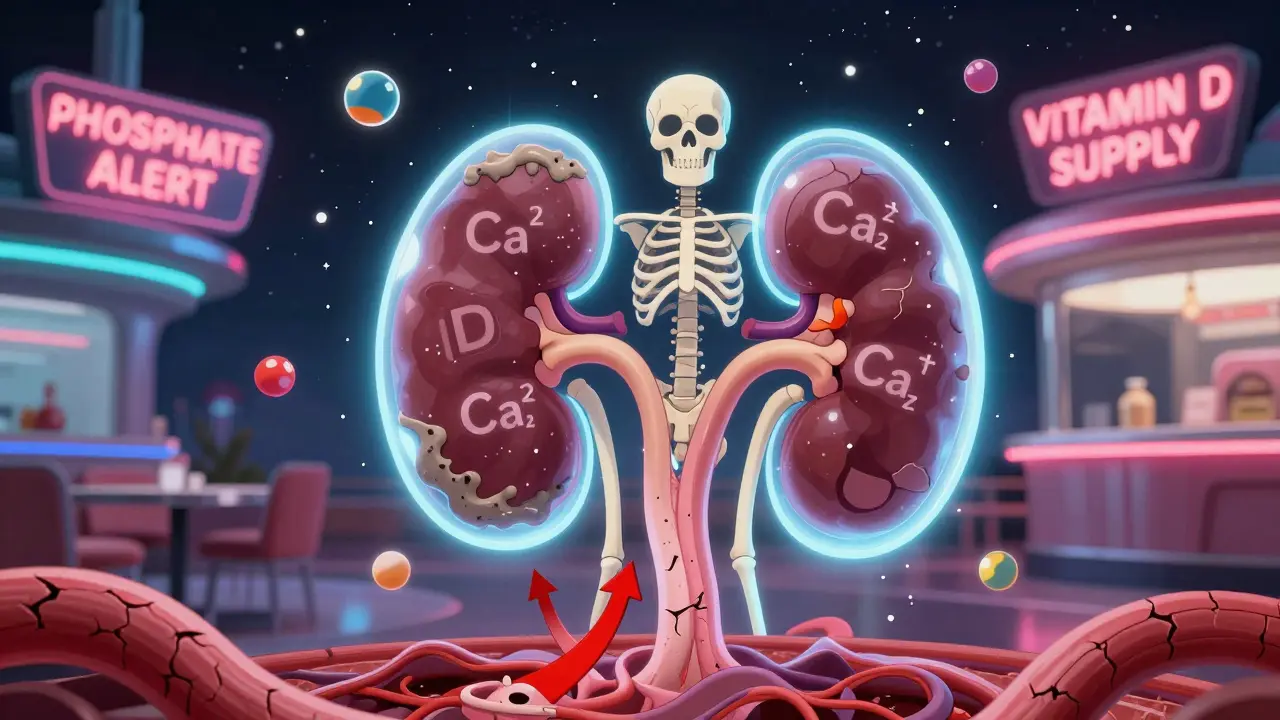
When your kidneys start to fail, they don’t just stop filtering waste. They also stop managing the minerals and hormones that keep your bones strong and your heart safe. This is where CKD-MBD - Chronic Kidney Disease-Mineral and Bone Disorder - comes in. It’s not just about weak bones. It’s about a broken system: calcium, phosphate, parathyroid hormone (PTH), and vitamin D all go haywire together. And if left unchecked, it can lead to fractures, heart attacks, and early death.
What Exactly Is CKD-MBD?
CKD-MBD isn’t a single problem. It’s a chain reaction. The Kidney Disease: Improving Global Outcomes (KDIGO) group defined it in 2006 to replace the outdated term ‘renal osteodystrophy,’ which only looked at bone damage. But here’s the truth: when your kidneys decline, your blood chemistry changes - and those changes hurt your heart, your bones, and your blood vessels.
By Stage 3 CKD (when your kidney filter rate drops below 60 mL/min), your body already starts struggling. Phosphate builds up because your kidneys can’t flush it out. That triggers a hormone called FGF23 to spike - sometimes 10 to 1000 times higher than normal. FGF23 tries to fix things by telling your kidneys to dump more phosphate. But as kidney function worsens, even FGF23 can’t keep up.
At the same time, your kidneys lose the ability to activate vitamin D. That means less calcitriol - the active form your body needs to absorb calcium from food. Low calcium then tricks your parathyroid glands into pumping out more PTH. Over time, these glands swell up and become overactive. This is called secondary hyperparathyroidism. But here’s the twist: even with high PTH, your bones stop responding well. It’s like shouting at a deaf person - the signal is there, but nothing happens.
The Calcium-PTH-Vitamin D Triangle
These three players - calcium, PTH, and vitamin D - are locked in a deadly dance.
- Calcium: Your target range is 8.4 to 10.2 mg/dL. Too low, and your parathyroid glands go into overdrive. Too high, and calcium starts sticking to your arteries, heart valves, and lungs.
- PTH: Normal levels are 10-65 pg/mL. In Stage 3 CKD, levels above 65 pg/mL signal trouble. By Stage 5D (dialysis), over 80% of patients have PTH above 300 pg/mL. But here’s the catch: high PTH doesn’t always mean your bones are breaking down. Sometimes, your bones become too quiet - a condition called adynamic bone disease - and that’s just as dangerous.
- Vitamin D: Over 80% of people with Stage 3-5 CKD are deficient in 25-hydroxyvitamin D. That’s not just a lab number - it’s linked to a 30% higher risk of dying. Your kidneys can’t turn vitamin D into its active form, so even if you take supplements, your body can’t use them properly.
These three don’t work in isolation. Low vitamin D → low calcium → high PTH → high phosphate → vascular calcification. Each step feeds the next. And once the cycle starts, it’s hard to break.
What Happens to Your Bones?
Bone disease in CKD isn’t one thing - it’s three.
- High turnover disease (osteitis fibrosa cystica): Seen in 20-30% of dialysis patients. PTH is sky-high - often over 500 pg/mL. Bones are constantly being broken down and rebuilt, but the new bone is weak. Fractures happen easily.
- Low turnover disease (adynamic bone disease): Now the most common type - affecting 50-60% of dialysis patients. PTH is low (under 150 pg/mL), and bone formation nearly stops. Your bones may look normal on a scan, but they’re brittle. This is often caused by too much calcium or too many phosphate binders.
- Mixed disease: A blend of both. Seen in 10-20% of cases. The bone is both overactive and underactive in different areas.
Here’s the scary part: dialysis patients have a 4 to 5 times higher risk of hip fractures than people their age without kidney disease. And because their bones are fragile, even a minor fall can be devastating.

What Happens to Your Heart and Blood Vessels?
Most people don’t realize that CKD-MBD isn’t just a bone problem - it’s a cardiovascular killer.
Calcium and phosphate, when out of balance, start depositing in your arteries. This is called vascular calcification. By Stage 5D, 75-90% of dialysis patients have it. Coronary artery calcification scores are 3 to 5 times higher than in healthy people. Each 1 mg/dL rise in phosphate means an 18% higher risk of death. Each 30% rise in PTH? A 12% higher risk.
These deposits make arteries stiff. Your heart has to work harder. Blood pressure spikes. Heart attacks and strokes become more likely. In fact, cardiovascular disease causes about half of all deaths in people on dialysis.
How Is It Diagnosed?
There’s no single test. Diagnosis is a puzzle made of blood tests, symptoms, and risk factors.
- Blood tests: Every 3-6 months, you need calcium, phosphate, PTH, and 25-hydroxyvitamin D checked. KDIGO recommends phosphate below 4.6 mg/dL for Stage 3-5 CKD, and 3.5-5.5 mg/dL for dialysis. PTH should be 2-9 times the upper limit of normal for your lab’s reference range. Vitamin D should be above 30 ng/mL.
- Bone biopsy: The gold standard for knowing what’s happening inside your bones. But it’s invasive. Only 5% of patients get one. Doctors usually guess based on PTH levels and bone markers like bone-specific alkaline phosphatase (BSAP) and PINP.
- Imaging: Plain X-rays can show moderate calcification. But CT scans (Agatston score) are far more accurate - detecting calcification in 90% of cases. Many centers now screen dialysis patients with CT scans every few years.
Don’t wait for symptoms. By the time you feel bone pain or chest tightness, the damage is often advanced.

Treatment: It’s Not Just About Pills
There’s no magic bullet. Treatment is layered and personal.
Phosphate Control
Phosphate is the trigger. Most people eat 1,200-1,500 mg a day - way over the 800-1,000 mg target for CKD.
- Diet: Avoid processed foods - they’re loaded with hidden phosphate additives. Colas, deli meats, frozen meals, and even some breads contain phosphate that your body absorbs fully. Stick to fresh meat, vegetables, and whole grains.
- Binders: These pills stick to phosphate in your gut so it doesn’t get absorbed. Calcium-based binders (like calcium carbonate) are cheap but risky - too much can cause calcification. Limit to 1,500 mg elemental calcium per day. Non-calcium binders like sevelamer or lanthanum are safer for your arteries but cost more.
Vitamin D
Start with nutritional vitamin D - cholecalciferol (D3). Take 1,000-4,000 IU daily to get your 25(OH)D above 30 ng/mL. This reduces death risk by 15% and doesn’t raise calcium or phosphate.
Active forms like calcitriol or paricalcitol? Only use them if PTH is above 500 pg/mL. They work fast but can spike calcium and phosphate. Use them like a scalpel - precise and cautious.
Calcium and PTH
Keep calcium in the safe zone. Avoid overusing calcium-based binders. If PTH stays high despite vitamin D and binders, consider a calcimimetic - cinacalcet or etelcalcetide. These drugs trick your parathyroid glands into thinking calcium is higher than it is. They can drop PTH by 30-50% without raising phosphate.
What About New Treatments?
Research is moving fast. Drugs that block sclerostin - a protein that shuts down bone building - are in trials. One, romosozumab, increased bone density by 30-40% in Stage 3-4 CKD patients. Another, etelcalcetide (a weekly injection), cuts PTH more than oral cinacalcet.
Even more exciting: scientists are testing Klotho protein supplements in animals. Klotho helps the kidneys handle phosphate and protects the heart. When given to mice with CKD, it cut vascular calcification by 50-60%. Human trials are coming.
The Big Picture: It’s All Connected
Doctors used to treat calcium, then PTH, then phosphate - one at a time. Now we know that’s like fixing one leak in a flooded house while ignoring the broken pipe.
CKD-MBD is a system failure. Treat the phosphate, and you help the PTH. Lower the PTH, and you protect the bones. Restore vitamin D, and you reduce death risk. Everything links back to everything else.
And it starts early. FGF23 rises years before phosphate does. That’s why KDIGO now recommends checking vitamin D and phosphate every 6-12 months starting at Stage 3 CKD - not just when you’re on dialysis.
What You Can Do Today
- Ask for your phosphate, calcium, PTH, and vitamin D levels - and ask what the targets are for you.
- Read food labels. Avoid ingredients with ‘phos’ in them - sodium phosphate, calcium phosphate, phosphoric acid.
- Take vitamin D3 daily. Don’t wait for your doctor to suggest it.
- Don’t take calcium supplements unless your doctor says so. Most people get enough from food.
- Ask if you need a bone density scan or vascular calcification screening - especially if you’re on dialysis.
CKD-MBD doesn’t have to be a death sentence. But it demands attention - early, consistent, and smart. Your bones and your heart are counting on it.
What are the signs of mineral bone disorder in kidney disease?
Early on, there are often no symptoms. By the time you feel bone pain, joint stiffness, or muscle cramps, damage may already be advanced. Some people notice itching, calcified lumps under the skin, or chest pain from hardened arteries. The real danger is silent - high phosphate and PTH levels can be killing your heart without you knowing.
Can vitamin D supplements help with CKD-MBD?
Yes - but only the right kind. Nutritional vitamin D (cholecalciferol or D3) helps restore low levels and lowers death risk by 15%. Active forms like calcitriol are powerful but risky - they can raise calcium and phosphate too much. Use them only if PTH is very high and under close supervision.
Why is phosphate so dangerous in kidney disease?
Your kidneys can’t remove excess phosphate. It builds up, triggers FGF23 and PTH spikes, and causes calcium to deposit in your arteries, heart valves, and lungs. Each 1 mg/dL rise in phosphate increases your risk of dying by 18%. Processed foods are the biggest hidden source - not dairy or meat.
Is bone biopsy necessary for diagnosing CKD-MBD?
No - but it’s the most accurate. Most doctors rely on blood tests (PTH, calcium, phosphate) and bone markers like BSAP or PINP. Bone biopsy is reserved for complex cases - like when treatment isn’t working or when low turnover disease is suspected. It’s invasive, so it’s not routine.
Can CKD-MBD be reversed?
Some damage can be slowed or stabilized - especially if caught early. Vascular calcification rarely reverses, but its progression can be cut in half with good phosphate control. Bone turnover can normalize with the right mix of vitamin D, calcimimetics, and avoiding over-treatment. The goal isn’t always full reversal - it’s preventing heart attacks and fractures.
Do children with CKD get mineral bone disorder too?
Yes - and it affects their growth. Children with Stage 5 CKD often have height Z-scores 1.5 to 2.0 standard deviations below normal. Their bones don’t grow right because of low vitamin D, high phosphate, and abnormal PTH. Early, aggressive treatment with vitamin D and phosphate binders is critical to help them reach normal height.
What’s the biggest mistake in treating CKD-MBD?
Treating one thing without seeing the whole picture. Giving too much calcium to fix low calcium? You might calcify the heart. Lowering PTH too much with drugs? You might cause adynamic bone disease. Aggressively cutting phosphate with binders? You might make patients malnourished. Balance is everything.

Lydia H.
January 20, 2026 AT 08:25Man, I read this whole thing and just sat there thinking about how nobody talks about this until it’s too late. I had a cousin on dialysis who never knew her arteries were turning to stone until she had a stroke. It’s wild how silent this stuff is.
Phil Hillson
January 20, 2026 AT 21:09this post is basically a textbook chapter but like… why do i care if my bones are weak if my heart’s already failing anyway
Valerie DeLoach
January 21, 2026 AT 01:24What struck me most isn’t just the science-it’s how the system fails people long before they even get diagnosed. In rural areas, getting blood tests every 3-6 months is a luxury. Many patients don’t even know what ‘PTH’ stands for. We need community health workers who can translate this into plain language-not just pamphlets in a clinic no one visits. This isn’t just medical-it’s social justice.
And yes, phosphate additives in processed food are a corporate conspiracy disguised as convenience. We’ve been sold a lie that cheap meals are affordable. They’re not. They’re killing us slowly, quietly, and disproportionately in low-income communities.
I’ve seen grandmas on dialysis avoid dairy because they’re told it’s high in phosphate, but they’re eating Pop-Tarts and canned soup daily. The real villain isn’t milk-it’s the food industry. We need policy change, not just pill regimens.
Also, vitamin D deficiency isn’t just a lab number-it’s a cultural one. In communities of color, darker skin means less synthesis. Yet guidelines rarely adjust for that. We’re treating symptoms while ignoring root causes rooted in equity.
And don’t get me started on bone biopsies. You need a specialist, a hospital, insurance approval, and a week off work. Meanwhile, your heart is calcifying. This system is designed for the privileged. The rest of us are just surviving.
But here’s hope: the new Klotho trials? That’s the kind of science that doesn’t just treat disease-it reimagines healing. Maybe one day, we won’t need to manage failure-we’ll prevent it.
Astha Jain
January 21, 2026 AT 07:07so phosphate is bad but like… i love soda so i guess i’m doomed lol
Josh Kenna
January 23, 2026 AT 00:54I’ve been on dialysis for 4 years and this is the first time someone explained why my bones hurt without sounding like a drug commercial. The part about adynamic bone disease? That’s me. My doctor kept lowering my PTH and now I can’t even lift my grandkid. I thought I was getting better. Turns out I was just… frozen. Please tell your docs to stop treating numbers and start treating people.
Lewis Yeaple
January 23, 2026 AT 22:28While the clinical correlations presented are largely accurate, the author's conflation of observational data with causal inference warrants caution. The association between serum phosphate levels and mortality, while statistically significant, may be confounded by nutritional status, inflammation, and residual renal function. Moreover, the assertion that 'each 1 mg/dL rise in phosphate increases risk by 18%' oversimplifies a multivariate relationship best modeled through Cox regression with time-dependent covariates.
Furthermore, the recommendation to screen for vascular calcification via CT scan in all dialysis patients lacks robust cost-effectiveness analysis. The American College of Radiology does not endorse routine screening absent symptomatic presentation.
While lifestyle modifications are prudent, the demonization of calcium-based binders ignores their proven efficacy in reducing hospitalization rates for hyperphosphatemia. A balanced, individualized approach remains paramount.
Jackson Doughart
January 25, 2026 AT 14:48I appreciate how this breaks down a complicated system into something digestible. But I wonder-how many of us are treating this like a checklist instead of a living process? My mom’s nephrologist gave her a 12-page handout and said ‘read this.’ She didn’t understand half of it. Maybe the real breakthrough isn’t new drugs-it’s better communication. We need doctors who sit down, not just send emails.
sujit paul
January 27, 2026 AT 06:27Let me tell you something the medical industry doesn’t want you to know: phosphate binders are just a cover-up. The real cause of CKD-MBD is fluoride in the water supply. It’s been proven in Japan, Russia, and even the CDC’s own archives. They don’t want you to know because Big Pharma profits from binders and calcimimetics. Drink spring water. Avoid fluoridated toothpaste. Your bones will thank you.
Also, vitamin D3 is a myth. The body only makes real vitamin D from sunlight-supplements are synthetic poison. Go outside. Let your skin breathe. That’s the ancient wisdom they erased.
Tracy Howard
January 29, 2026 AT 05:50Can we just admit that American processed food is the real epidemic? I came here from Canada and I was shocked-every single grocery store aisle is poison. We don’t have this problem up north because we actually regulate additives. You think this is about kidneys? No. It’s about corporate greed and lazy policy. And now you’re telling me we’re supposed to eat ‘fresh meat and vegetables’ when a family of four on minimum wage can’t afford it? This isn’t medicine. It’s class warfare.
Aman Kumar
January 29, 2026 AT 10:13The pathophysiology of CKD-MBD is a quintessential example of systemic dysregulation within the endocrine-renal axis. The FGF23-Klotho axis represents a maladaptive compensatory mechanism that, in its persistence, engenders iatrogenic harm via vascular calcification and adynamic bone disease. The clinical paradigm remains reductionist-fixing calcium, then PTH, then phosphate-when the true imperative lies in restoring homeostatic equilibrium at the molecular level. We are treating symptoms, not the ontological rupture of mineral metabolism.
Moreover, the absence of biomarker-guided precision therapy reflects a fundamental epistemological failure in nephrology. Until we embrace multi-omics profiling and machine learning-driven phenotyping, we remain in the Stone Age of renal medicine.
Jake Rudin
January 30, 2026 AT 07:46Interesting. But I think the real issue is the lack of longitudinal data on FGF23 trajectories in early-stage CKD. We’ve got cross-sectional studies galore, but who’s tracking patients from Stage 2 to Stage 5? Without that, we’re just guessing at causality. Also-why is everyone so obsessed with phosphate? What about magnesium? It’s a natural calcium blocker, and we barely test for it. And why isn’t anyone talking about the gut-kidney axis? Microbiome changes alter phosphate absorption. This feels like we’re missing half the puzzle.
Erwin Kodiat
January 30, 2026 AT 15:48My dad’s on dialysis. He started taking D3 supplements last year. His phosphate didn’t drop, but his energy did. He’s walking again. He doesn’t talk about it much, but I see him smiling now. Maybe it’s not about fixing everything. Maybe it’s just about giving people back a little dignity.
Christi Steinbeck
January 31, 2026 AT 02:59Stop waiting for your doctor to tell you what to do. Go get your labs. Learn what the numbers mean. Buy a food scale. Read labels like your life depends on it-because it does. I did this for my mom. She’s 72. Still alive. Still gardening. Still here. It’s not magic. It’s just showing up.
Jacob Hill
February 1, 2026 AT 01:50I’ve been reading everything I can on this since my brother passed last year. I didn’t know phosphate additives were in bread. I didn’t know PTH could be too low. I didn’t know my family’s diet was slowly killing him. I’m telling everyone I know now. This isn’t just a kidney thing. It’s a family thing. A community thing. A wake-up call.
Malikah Rajap
February 1, 2026 AT 20:11Can we talk about how the word ‘adynamic’ sounds like a villain in a sci-fi movie? Like, ‘The Adynamic Bone Disease has taken over the kidneys!’ Anyway-I’ve been taking sevelamer for two years and my PTH dropped from 800 to 180. No more bone pain. No more itching. But my doctor still won’t stop my calcium pills. I’m scared. Can someone tell me if I’m doing this right?