Personalized Medication Risk Calculator
How Your Body Processes Medications
This tool estimates your risk of adverse drug reactions based on key factors discussed in the article. Enter your information to see personalized insights.
Personalized Risk Assessment
Have you ever taken the same medication as someone else-same dose, same condition-and had a totally different experience? One person feels fine, while another ends up in the hospital. It’s not luck. It’s biology. Medications don’t work the same way for everyone, and the reasons go far beyond "you’re just sensitive." The truth is, your genes, your age, your other meds, even your gut bacteria, are all quietly deciding how your body handles every pill you swallow.
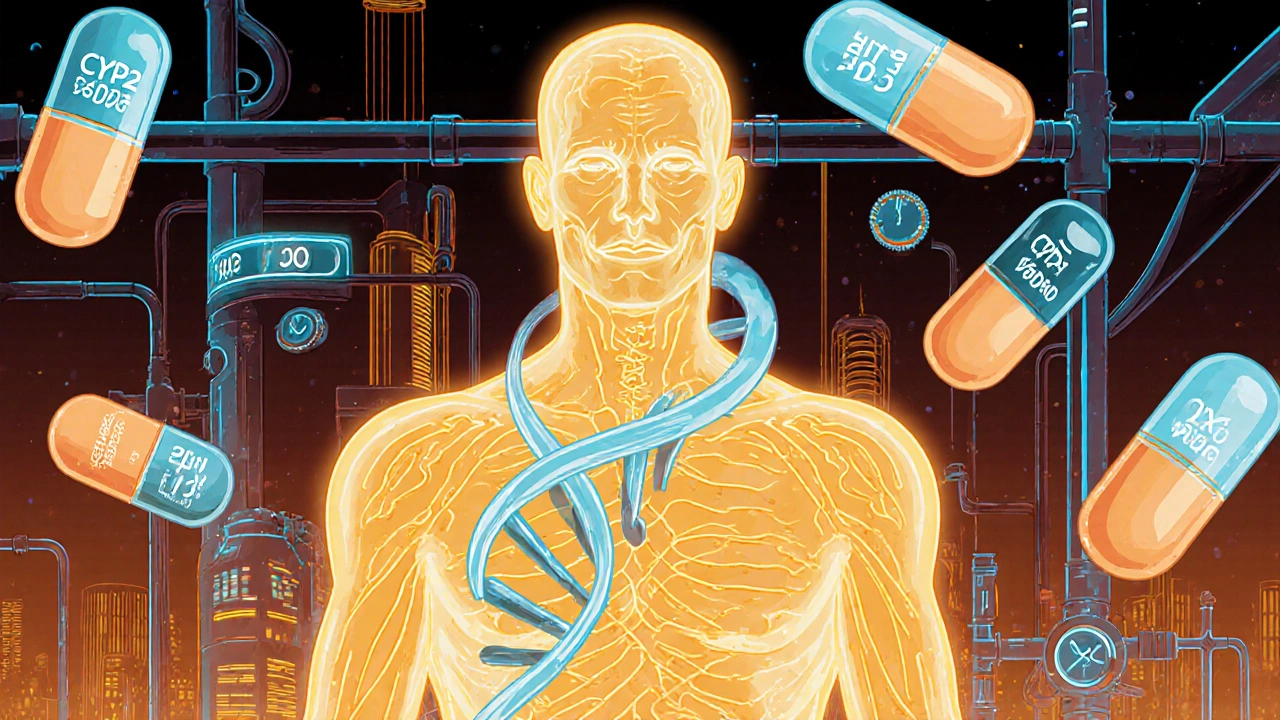
It’s Not Just You-It’s Your Genes
Your DNA is the biggest factor in how you react to drugs. Some people are born with versions of genes that make them break down medications too fast, too slow, or not at all. The most common culprits are enzymes called cytochrome P450, especially CYP2D6, CYP2C9, and CYP2C19. These are like your body’s drug-processing machines. If your machine is broken or overpowered, the drug either builds up to dangerous levels or gets washed out before it can work.
For example, about 5 to 10% of white people are "poor metabolizers" of CYP2D6. That means drugs like codeine, antidepressants, or beta-blockers stay in their system way too long. On the flip side, up to 29% of Ethiopians are "ultra-rapid metabolizers"-they process these drugs so quickly, the medicine doesn’t even have time to help. A person with this profile might take a standard dose of codeine and get no pain relief, while someone else with the same dose could overdose because their body turns it into morphine too fast.
This isn’t theoretical. In 2022, a Mayo Clinic study tracked 10,000 patients. Those who got genetic testing before starting certain drugs had 32% fewer emergency room visits and 26% shorter hospital stays. That’s not a small win-it’s life-changing.
Age Changes Everything
As you get older, your body changes. Fat increases. Muscle decreases. Your liver and kidneys don’t filter things the way they used to. That means drugs that were perfectly safe at 30 can become risky at 70.
Take sleeping pills or anti-anxiety meds. These are fat-soluble. Older adults naturally have more body fat-up to 30-40% more than young adults. So these drugs stick around longer, building up in the system. One study found elderly patients were 300% more likely to suffer dangerous side effects from these drugs than younger people. And it’s not just sedatives. Blood thinners like warfarin? Older patients need much lower doses. Too high, and you risk a bleed. Too low, and you’re unprotected from clots.
That’s why doctors often start seniors on half-doses. It’s not being cautious-it’s basic science.
Other Medications Are Playing Hide and Seek
Most people aren’t taking just one drug. The average American over 65 takes five or more prescriptions. That’s a recipe for hidden conflicts.
Take amiodarone, a heart rhythm drug. It blocks the enzyme that breaks down warfarin. When taken together, warfarin levels can spike by 100 to 300%. That’s not a minor interaction-it’s a bleeding risk. One 68-year-old woman in a JAMA case study kept having dangerous INR spikes (above 10, when normal is 2-3). Her doctors couldn’t figure it out-until genetic testing revealed she was a CYP2C9*3/*3 poor metabolizer. Her warfarin dose had to be cut by 60%.
NSAIDs like ibuprofen or naproxen cause stomach ulcers in 1-2% of users. But if you also take steroids and have a certain genetic variant, your risk jumps to 15-30%. That’s not a coincidence. That’s a perfect storm of genes and drugs.
Why We’re Still Guessing-And What’s Changing
Despite knowing all this, most doctors still prescribe based on weight, age, and symptoms-not genetics. Why? Because testing isn’t routine. Only 18% of U.S. insurers cover pharmacogenomic tests. Only 32% of hospitals have systems that automatically flag dangerous gene-drug combos in electronic records. And 68% of physicians say they don’t feel trained to use the results.
But things are shifting. The FDA now lists pharmacogenomic info for over 300 drugs, with specific dosing guidance for 44 of them. Medicare started covering genetic tests for 17 high-risk medications in January 2024. In oncology, 65% of hospitals use pharmacogenomics routinely. At St. Jude Children’s Research Hospital, testing for mercaptopurine (a leukemia drug) cut severe side effects from 25% to 12%.
And it’s not just about single genes anymore. Researchers are now building polygenic risk scores-combining hundreds of genetic signals to predict how someone will respond. Early data shows these scores are 40-60% more accurate than single-gene tests.
What This Means for You
If you’re on multiple medications, especially if you’re over 65 or have had unexpected side effects, ask your doctor about pharmacogenomic testing. It’s not a magic bullet, but it’s the closest thing we have to personalized medicine today.
You don’t need to get tested for everything. Focus on drugs where genetics matter most: blood thinners (warfarin), antidepressants, painkillers (codeine, tramadol), anti-seizure meds, and certain cancer treatments. If you’ve had a bad reaction to a drug before-even if it was mild-genetic testing might explain why.
And if you’re a caregiver for an older relative? Pay attention to new symptoms after a medication change. Dizziness, confusion, bruising, or stomach pain could be signs of a drug-gene interaction, not just "getting older."
The Future Is Personalized-But It’s Not Here Yet
The goal is simple: no more guessing. No more trial and error. No more preventable hospitalizations. Pharmacogenomics isn’t science fiction-it’s already saving lives in hospitals across the country. But it’s still stuck in the slow lane for most people.
Costs have dropped from $2,000 per test in 2015 to under $250 today. The science is solid. The data is clear. What’s missing is access. Until testing becomes standard, part of your job as a patient is to ask the right questions. Don’t assume your doctor knows your genetic profile. Most don’t. But you can start the conversation.
Because when it comes to your health, one size never did fit all. And now, we finally have the tools to prove it.
Why do some people get side effects from drugs that others don’t?
It’s mostly due to genetic differences-especially in enzymes like CYP2D6 and CYP2C19 that break down drugs. Some people metabolize medications too slowly, causing buildup and toxicity. Others process them too fast, making the drug ineffective. Age, other medications, liver and kidney function, and even diet can also change how your body handles drugs.
Is genetic testing for drug reactions worth it?
For certain high-risk drugs-like warfarin, clopidogrel, antidepressants, or codeine-yes. Studies show genetic testing can reduce emergency visits by 32% and hospital stays by 26%. It’s especially valuable if you’ve had unexpected side effects before, take multiple medications, or are over 65. Costs are now under $250, and Medicare covers it for 17 key drugs starting in 2024.
Can my doctor test me for drug gene interactions?
Many can, but not all do. Ask if your doctor uses pharmacogenomic testing or if your hospital has a pharmacogenomics program. If not, you can request a test through a specialist, genetic counselor, or direct-to-consumer service (though always share results with your doctor). The FDA has labeled over 300 drugs with genetic guidance, so your doctor should be able to find relevant info.
What drugs are most affected by genetic differences?
Warfarin (blood thinner), clopidogrel (antiplatelet), antidepressants like SSRIs, opioids like codeine and tramadol, statins (cholesterol drugs), and certain cancer meds like mercaptopurine. These have well-documented gene-drug links. For example, 2-15% of people have a CYP2C19 variant that makes clopidogrel useless for preventing heart attacks.
Are side effects from medications common?
Very. In Europe, 3.6% of hospital admissions are due to adverse drug reactions. In the U.S., ADRs are the fourth leading cause of death. NSAIDs cause stomach problems in 1-2% of users yearly-but that jumps to 15-30% in people with certain genes and those taking steroids. The real number is likely higher because many side effects are blamed on aging or other conditions.
Can I avoid side effects without genetic testing?
Yes, but less reliably. Start with the lowest effective dose. Tell your doctor every medication and supplement you take-even herbs and OTC painkillers. Report even mild side effects. Avoid alcohol with sedatives or pain meds. Stay hydrated. But if you’ve had unexplained reactions before, testing gives you real answers-not just guesswork.

Alex Harrison
November 8, 2025 AT 09:37I’ve been on warfarin for years and never knew my genes could be why my INR keeps jumping. My doctor just kept tweaking the dose like it was a game of darts. Turns out I’m a CYP2C9*3/*3 carrier-no wonder I almost bled out last winter. This article finally explains why I’ve been walking on eggshells for a decade.
Jay Wallace
November 9, 2025 AT 06:39Of course it’s genetics. America’s entire medical system is built on guesswork because we’re too lazy to test people. In Germany, they screen everyone before prescribing SSRIs. Here? We just throw pills at people and hope they don’t die. Pathetic. And don’t even get me started on how the FDA’s slow to act. We’re literally losing people to ignorance.
Alyssa Fisher
November 10, 2025 AT 00:01It’s fascinating how biology doesn’t care about our assumptions. We treat medicine like a one-size-fits-all software update, but the human body is a living ecosystem-genes, microbiome, age, diet, even stress levels all interact in ways we’re only beginning to map. This isn’t just about avoiding side effects; it’s about recognizing that health isn’t a formula, it’s a conversation between your biology and the drugs you take.
Alyssa Salazar
November 10, 2025 AT 06:23Let’s be real-pharmacogenomics is the future, and anyone who isn’t pushing for universal access is complicit in preventable harm. We’ve got polygenic risk scores that outperform single-gene tests by 60%, yet most docs still prescribe based on weight and guesswork. This isn’t innovation lagging-it’s systemic negligence. Insurance won’t cover it? Fine. We need to demand it. Hospitals need to build EHR alerts. Patients need to stop being passive recipients and start demanding data-driven care.
Beth Banham
November 11, 2025 AT 16:35I’m 71 and on five meds. My grandkids keep telling me to ask about genetic testing, but I’m scared to rock the boat. Still… I did have that weird dizziness after starting the new blood pressure pill. Maybe I should bring it up next visit. Thanks for the nudge.
Brierly Davis
November 12, 2025 AT 22:42Big shoutout to everyone pushing for this stuff. Seriously. I had a cousin who took codeine after surgery and went into respiratory arrest. Turns out she was an ultra-rapid metabolizer. If they’d tested her, she’d be alive today. Don’t wait for a tragedy. Ask your doc. Get tested. It’s not expensive anymore. You’ve got nothing to lose but unnecessary risk.
Amber O'Sullivan
November 14, 2025 AT 07:27My mum’s on statins and antidepressants and she’s always been weirdly tired. No one ever connected it. Now I’m reading this and thinking maybe it’s her CYP2D6. I’m ordering a test this week. No more guessing
Jim Oliver
November 16, 2025 AT 04:03Oh wow. Another article that blames doctors for not being mind readers. Did you forget that 68% of physicians say they’re not trained? Maybe instead of shaming them, we should fix the training. Or maybe you’re just mad because your grandma’s prescription didn’t magically become perfect after reading this.
William Priest
November 17, 2025 AT 10:47Look, if you’re not running a polygenic risk score before every Rx, you’re basically playing Russian roulette with your liver. I’ve seen people on 300mg of venlafaxine because their doc didn’t know about CYP2D6. That’s not medical care. That’s negligence dressed up as tradition.
Ryan Masuga
November 17, 2025 AT 23:21My aunt got tested after a bad reaction to an antidepressant and they switched her to one that matched her profile. She’s been sleeping through the night for the first time in 15 years. It’s not magic. It’s science. And it’s available. You just gotta ask. Don’t be shy-your life’s worth it.
Jennifer Bedrosian
November 18, 2025 AT 02:23I had a panic attack after taking tramadol and everyone thought I was just anxious but now I know I’m a CYP2D6 ultra-rapid metabolizer and my body turned it into morphine like a factory. I cried reading this. Finally someone gets it. I’m not crazy. My genes are just evil
Lashonda Rene
November 18, 2025 AT 19:08I never thought about how my gut bacteria could be changing how my meds work. I mean, I eat yogurt and probiotics and stuff but I didn’t realize that could affect whether a drug even works or not. I guess I need to stop thinking of my body like a car that just needs the right fuel and start thinking of it like a whole garden that’s got its own little ecosystem. It’s kind of wild when you think about it.
Andy Slack
November 19, 2025 AT 07:05Just got my 23andMe results back. Found out I’m a CYP2C19 poor metabolizer. Took me 3 years to figure out why Plavix didn’t work. Now I’m telling every family member to get tested. This is the most important health info I’ve ever had.
Rashmi Mohapatra
November 19, 2025 AT 11:52Everyone in India knows this already. We’ve been doing pharmacogenomics for decades because we can’t afford to waste money on drugs that don’t work. You Americans think you’re advanced but you’re still guessing. Pathetic.