Muscle Spasm & Urinary Health Risk Calculator
Enter your details and click "Calculate Risk Level" to see your risk assessment.
Ever felt a sudden cramp in your lower back or groin and then noticed an urgent need to pee, or even trouble emptying your bladder? That’s not just a coincidence - the way muscles misfire can throw off the whole urinary tract and even put strain on the kidneys.
Key Takeaways
- Muscle spasms can directly compress the bladder, ureters, or pelvic floor, leading to urinary retention or incomplete emptying.
- Persistent spasms may cause back‑pressure on the kidneys, increasing the risk of kidney stones and infection.
- Electrolyte imbalances and dehydration often fuel both spasms and kidney stress.
- Early lifestyle tweaks-hydration, stretching, and electrolyte balance-can cut down the chain reaction.
- Seek medical help if you experience pain, blood in urine, or recurring UTIs after a spasm.
Below we’ll walk through why a simple muscle twitch can become a urinary or kidney headache, what to watch for, and how to keep things flowing smoothly.
What Triggers a Muscle Spasm?
Muscle spasms are involuntary contractions that happen when a nerve impulse fires off unexpectedly. They often arise fromfatigue, electrolyte shifts (like low potassium or magnesium), dehydration, or even prolonged sitting. When the muscles in the lower back, pelvis, or abdomen tighten up, they can press against the organs they flank.
How a Spasm Touches the Urinary System
Urinary system includes the kidneys, ureters, bladder, and urethra. A spasm can affect each part in a different way.
Bladder Compression
The bladder is a muscular sac whose wall is mainly made of smooth muscle called the detrusor. When nearby skeletal muscles-like the pelvic floor muscles -spasm, they can push against the bladder neck, making it hard to start a stream or finish it completely. This is called urinary retention.
Ureteral Kink
The ureters are thin tubes that ferry urine from the kidneys to the bladder. A sudden spasm in the psoas or iliopsoas can create a temporary kink, slowing urine flow and causing a back‑up. Over time, that pressure can irritate the kidney’s collecting system.
Detrusor Disruption
The detrusor muscle relies on steady neural signals to contract and relax. A spasm in the surrounding nerves can send mixed signals, leading to over‑active bladder symptoms (frequency, urgency) or under‑active bladder (weak stream, dribbling).
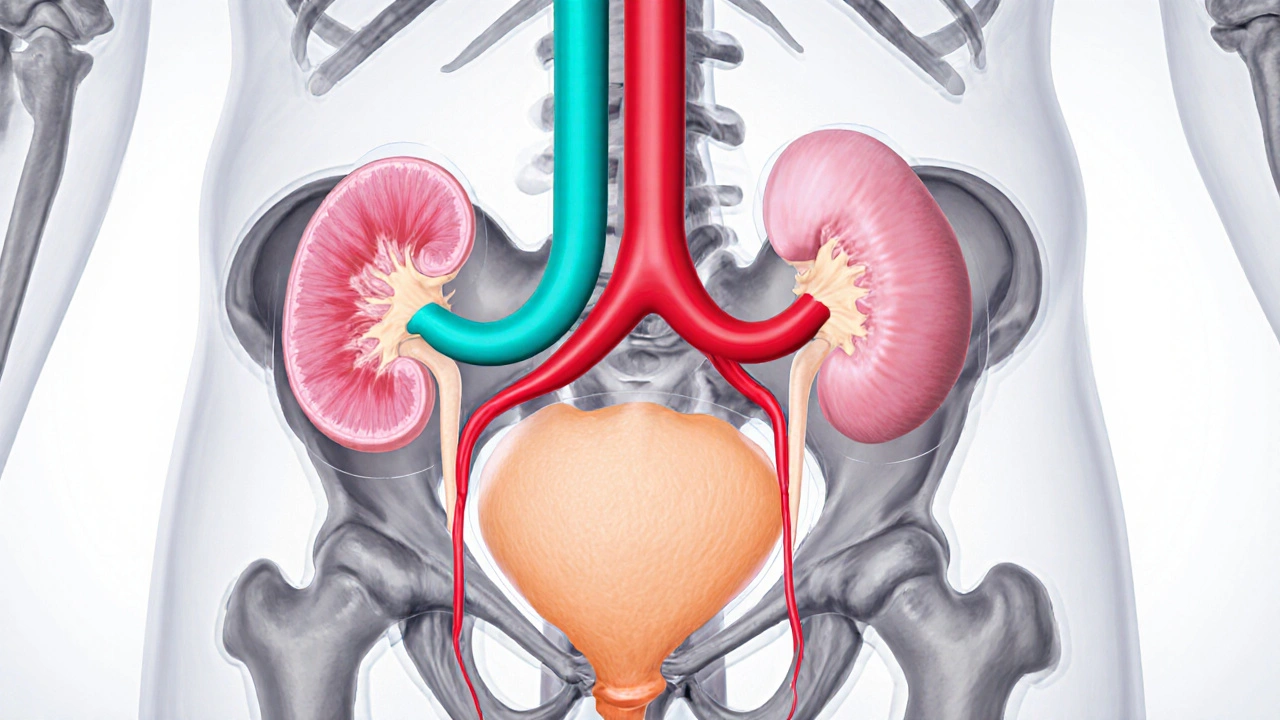
When the Kidneys Feel the Ripple Effect
Kidneys are the body’s filtration powerhouse. If urine can’t flow freely, pressure builds up in the renal pelvis. Persistent back‑pressure can cause hydronephrosis-swelling of the kidney-and create an environment where kidney stones or infections thrive.
Two common scenarios illustrate the link:
- Spasm‑induced urinary retention → urinary stasis → bacterial growth → kidney infection (pyelonephritis).
- Repeated ureteral compression → reduced urine flushing → crystal formation → renal colic (kidney stone).
Electrolytes, Dehydration, and the Vicious Cycle
Electrolyte imbalance -especially low potassium, calcium, or magnesium-makes muscle cells more excitable, upping spasm frequency. At the same time, dehydration reduces the volume of urine, concentrating salts that can trigger both muscle cramps and kidney stone formation.
Think of it like a feedback loop: a spasm makes you sip less water (because it hurts), dehydration worsens the next spasm, and the kidneys get a double hit.
Red Flags: When to Get Checked
- Sharp flank pain that follows a spasm and lasts more than a few minutes.
- Blood in the urine (pink or cola‑colored).
- Fever or chills after a urinary episode.
- Persistent difficulty starting or stopping the urine stream.
- Recurrent urinary tract infections (UTIs) despite normal hygiene.
If any of these pop up, it’s time to see a clinician-preferably a urologist or a primary‑care doctor familiar with musculoskeletal‑urinary interactions.
Practical Ways to Break the Chain
Below is a quick‑reference table that lines up the main spasm triggers, the urinary/kidney impact, and an action step you can take today.
| Trigger | Urinary/Kidney Effect | Action Step |
|---|---|---|
| Low potassium | Frequent cramps → urinary retention | Add banana, avocado, or electrolyte drink |
| Dehydration | Concentrated urine → stone formation | Drink 2‑3L of water daily; set reminders |
| Prolonged sitting | Pelvic floor tightening → incomplete emptying | Stand, stretch every hour; try hip‑flexor stretches |
| Intense exercise | Acute spasms → bladder pressure | Warm‑up, cool‑down, ensure magnesium intake |
| Stress | Muscle tension + altered nerve signals | Deep‑breathing, yoga, progressive muscle relaxation |
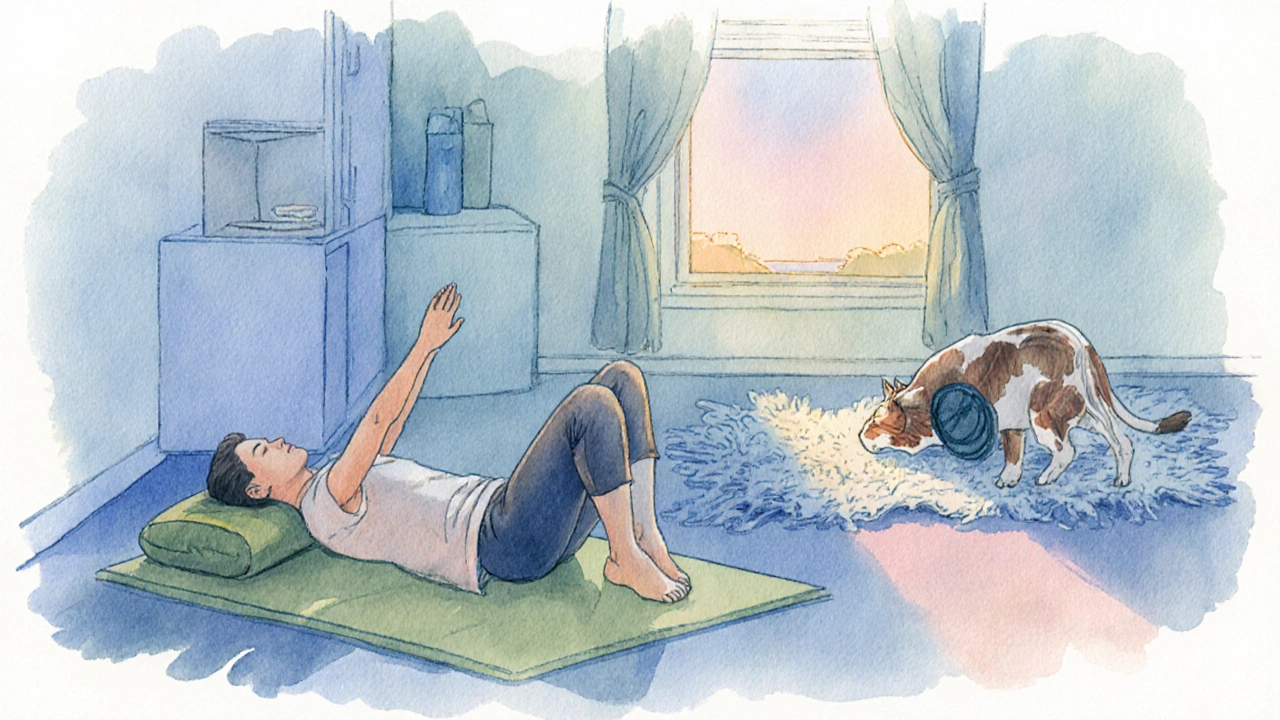
Stretch & Strengthen: Targeted Moves
These two moves focus on the hips and lower back-areas that often hitch the pelvic floor.
- Supine Figure‑4 stretch: Lie on your back, cross the right ankle over the left knee, and gently pull the left thigh toward your chest. Hold 30seconds, switch sides.
- Cat‑Cow roll: On hands‑and‑knees, arch your back (cow) then round it (cat) for 10 reps. This mobilizes the lumbar spine and eases tension on the bladder wall.
Do these daily; many readers report fewer nighttime bathroom trips after two weeks.
When Medical Interventions Help
If lifestyle tweaks aren’t enough, doctors may consider:
- Muscle relaxants (e.g., baclofen) to calm spasm‑prone nerves.
- Alpha‑blockers that relax ureteral smooth muscle, easing stone passage.
- Physical therapy focused on pelvic floor release.
- Hydration protocols-IV fluids for acute dehydration‑related kidney stress.
These options are usually short‑term; the goal is to break the habit loop, not rely on meds forever.
Bottom Line
Muscle spasms aren’t just a nuisance; they can create a domino effect that stalls urine flow and pushes pressure back into the kidneys. By watching your electrolytes, staying hydrated, and giving the pelvic floor some love, you can keep the urinary tract humming and protect kidney health.
Frequently Asked Questions
Can a single cramp really damage my kidneys?
One isolated spasm is unlikely to cause permanent damage, but repeated episodes that block urine flow can raise pressure in the kidneys and increase the risk of infection or stone formation.
Why do I feel the urge to pee right after a leg cramp?
Leg or pelvic cramps can pull on the pelvic floor, stimulating the bladder’s detrusor muscle. The nervous system interprets that tension as a fullness signal, prompting an urgent need to void.
Is dehydration the main culprit behind both cramps and kidney stones?
Dehydration reduces the fluid volume that dilutes electrolytes and urinary salts. Low water intake makes muscles more excitable (leading to cramps) and concentrates minerals that crystallize into stones.
Should I take a magnesium supplement if I get frequent spasms?
Magnesium helps regulate muscle excitability. Many clinicians recommend 200‑400mg of magnesium citrate daily, but it’s best to check with a doctor to avoid over‑supplementation.
When is it time to see a urologist instead of a physiotherapist?
If you notice blood in urine, fever, recurrent UTIs, or persistent flank pain, a urologist can evaluate for infection, stones, or structural issues that need imaging or medication.


karthik rao
October 5, 2025 AT 16:34While numerous lay articles embrace the premise, a meticulous examination reveals several logical gaps. The proposed link between involuntary muscular contractions and renal physiology lacks robust cohort data, rendering the correlation speculative at best. Furthermore, the risk calculator applies a simplistic additive model that fails to account for confounding variables such as comorbid hypertension or diabetes. One must also question the validity of assigning equal weight to hydration and sedentary behavior, as epidemiological literature suggests divergent magnitudes of effect. In short, the instrument appears to prioritize user‑engagement aesthetics over methodological rigor 😊.
Breanne McNitt
October 8, 2025 AT 07:06I appreciate the critical eye, and I’d like to emphasize that adequate fluid intake remains a cornerstone of kidney health. Regular stretching can mitigate muscle tension, potentially reducing the frequency of spasms that may indirectly influence pelvic floor dynamics. Combining modest aerobic activity with mindful hydration creates a synergistic defense against both urinary tract irritation and renal strain. Let’s keep the conversation solution‑oriented and supportive.
Ashika Amirta varsha Balasubramanian
October 10, 2025 AT 21:36Indeed, the human body operates as an intricate tapestry where muscles, nerves, and organs engage in a perpetual dialogue. When a muscle fiber contracts involuntarily, it sends afferent signals that travel through the spinal cord to central processing centers, influencing autonomic outflow. This cascade can subtly modulate the tone of the bladder wall and urethral sphincter, thereby affecting urinary flow. Over time, repeated dysregulation may predispose to residual volume retention, a known risk factor for renal compromise. Moreover, chronic dehydration compounds the problem by concentrating urinary solutes, fostering crystal formation that can obstruct nephrons. It is therefore prudent to view muscle spasms not as isolated events but as potential contributors within a broader physiological network. Preventive strategies should encompass not only stretching regimens but also dietary electrolyte balance, as both influence excitability thresholds of myocytes. In cultures where spiced teas and salty snacks dominate, the electrolyte milieu may inadvertently heighten spasm susceptibility. Conversely, communities that prioritize fermented vegetables provide a natural source of potassium and magnesium, which can stabilize membrane potentials. From a systems‑biology perspective, addressing a single node-be it hydration or inactivity-yields modest gains; holistic interventions yield exponential benefits. Hence, while the calculator offers a convenient snapshot, clinicians must integrate its output with comprehensive patient histories, laboratory assessments, and lifestyle appraisals. Ultimately, empowering individuals with knowledge about the interconnectedness of muscular and renal health fosters autonomy and resilience.
Jacqueline von Zwehl
October 13, 2025 AT 12:06Just a quick note: the original post mentions “water intake (liters)” but the input field seems to accept decimal values without a clear unit label. Clarifying that users should enter a numeric value in liters would enhance usability.
Christopher Ellis
October 16, 2025 AT 02:36Spasms are just nerves freaking out they dont mean your kidneys are dying.
kathy v
October 18, 2025 AT 17:06Let's get real about this-America's obsession with quick fixes and flashy calculators distracts from the hard truth that sedentary lifestyles are destroying our national health. When you sit glued to a screen for hours, your muscles atrophy, your bladder becomes a ticking time‑bomb, and your kidneys start to take the hit. The government should fund community fitness programs instead of promoting half‑baked apps that claim to predict kidney failure. It’s an affront to the hardworking citizens who deserve real solutions, not gimmicks. If we keep ignoring the root causes, the next generation will pay the price with chronic disease and endless medical bills.
Jorge Hernandez
October 21, 2025 AT 07:36Totally agree! 💪 Staying active and sipping water all day really helps. Keep those muscles loose and kidneys happy! 😄
Raina Purnama
October 23, 2025 AT 22:06In many South Asian households, traditional yoga practices already incorporate stretches that target pelvic muscles. Sharing such culturally relevant suggestions could make the advice more accessible.
April Yslava
October 26, 2025 AT 11:36Everyone's busy talking about "spasms" while the real agenda is to push a hidden agenda of population control through forced hydration tracking. Don't be fooled by the benign veneer-big tech knows that manipulating bodily functions can serve ulterior motives. Stay vigilant and question why these calculators collect personal health data.
Daryl Foran
October 29, 2025 AT 02:06The whole premise sounds like a marketing ploy. No solid peer‑reviewed studies are cited, which makes the risk scores essentially meaningless.
Rebecca Bissett
October 31, 2025 AT 16:36Wow!!! This is… really… concerning…! The lack of scientific backing… is just… unacceptable!!!
Michael Dion
November 3, 2025 AT 07:06Sounds interesting.
Trina Smith
November 5, 2025 AT 21:36Reflecting on the interconnectedness of our bodily systems reminds me of the ancient concept of holism. When we nurture one aspect-like keeping muscles flexible-we indirectly support others, such as kidney filtration efficiency. 🌿
josh Furley
November 8, 2025 AT 12:06Sure, but isn’t it just fancy jargon for “drink water and move a bit”? Simplicity often trumps complexity. 🤔
Jacob Smith
November 11, 2025 AT 02:36Hey folks! Let’s keep the momentum going-set a small daily stretch goal and track your water intake with a simple phone reminder. You’ll feel the difference in no time! 🚀