Most people think osteoarthritis is just aging joints wearing out. That’s not true. It’s not your bones grinding down like old gears. It’s a full-system failure inside your joint - cartilage, bone, ligaments, even the fluid that lubricates it all. And it’s happening to 32.5 million adults in the U.S. right now. The pain isn’t random. The stiffness isn’t just "getting older." This is a real, measurable disease - and the good news is, you can stop it from getting worse.
What’s Really Happening Inside Your Joint?
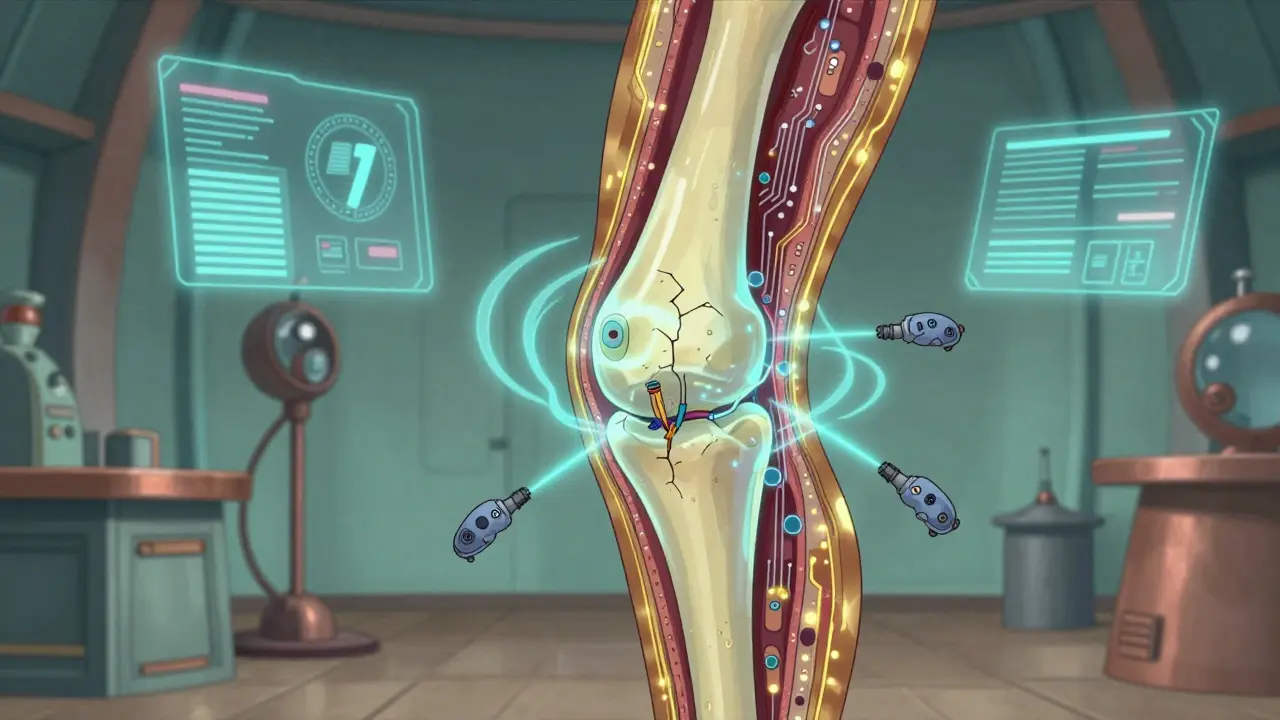
Your joints aren’t just bone on bone. They’re cushioned by articular cartilage - a smooth, slippery tissue that lets bones glide without friction. In osteoarthritis, that cartilage doesn’t just thin out. It breaks down in patches. Tiny cracks form. The surface gets rough. Chondrocytes - the cells that maintain cartilage - go into overdrive trying to fix it, but they end up making things worse. They release enzymes that chew up more cartilage. The bone underneath starts to thicken and grow spurs. The synovial fluid gets thin and sticky. Ligaments loosen. Even the fat around the joint starts releasing inflammatory chemicals.
This isn’t a slow fade. It’s a cycle: damage triggers inflammation, inflammation causes more damage, and the joint slowly loses its ability to move normally. That’s why pain gets worse with activity - you’re stressing a damaged system. And why rest helps - you’re giving it a break from the strain.
It usually hits the knees first - about 60% of cases. Then hips, hands, and spine. And it doesn’t hit both sides evenly. One knee might be fine, the other screaming. That’s not a coincidence. It’s often tied to past injuries, uneven posture, or how you move.
Osteoarthritis vs. Other Arthritis: It’s Not the Same
People mix up osteoarthritis with rheumatoid arthritis (RA) all the time. But they’re totally different. RA is an autoimmune disease. Your immune system attacks your joints. It causes swelling, heat, and morning stiffness that lasts for hours. Pain from RA often gets better with movement.
Osteoarthritis? No immune system involvement. No redness. No all-day swelling. Pain builds up during the day - walking, climbing stairs, standing too long. It eases when you sit down. Morning stiffness? Usually lasts less than 30 minutes. And it’s not symmetrical. One hand hurts, the other doesn’t.
Gout is another common confusion. That’s sudden, burning pain - often in the big toe - with visible redness and swelling. It’s caused by uric acid crystals. OA? No crystals. Just slow, steady breakdown.
Post-traumatic arthritis? That’s OA that starts after a serious injury - a torn ligament, a broken bone. It can show up years later. So if you hurt your knee in college and now it aches at 45, that’s likely not "just aging."
Why Most People Don’t Get Diagnosed Until It’s Too Late
OA sneaks up. At first, you just feel a little stiffness after sitting too long. Or your knee clicks when you stand up. You think, "I’m getting old." You ignore it. By the time you see a doctor, the cartilage is already significantly worn down. X-rays - the standard tool - only show damage after it’s advanced. That’s why experts like Dr. Virginia Byers Kraus say we’re diagnosing OA too late. We need better blood tests or imaging that catches early changes.
And here’s the catch: the pain doesn’t always match the damage. Some people with severe X-ray findings feel almost no pain. Others with mild changes are in constant agony. That’s why doctors rely on symptoms - not just images - to make a diagnosis.
The Real Treatment Plan: 4 Things That Actually Work
There’s no cure. But you don’t need one. You need a plan. And the best plan doesn’t start with pills. It starts with movement, weight, and education.
- Exercise - 3 times a week, minimum. Not running. Not heavy lifting. Walking, cycling, swimming, tai chi. The Arthritis Foundation found that people who stuck with 45-minute sessions three times a week saw 80% improvement in pain after 12 weeks. Strength training matters too - strong muscles take pressure off your joints. A 2023 study showed that targeted physical therapy with 6-8 sessions improved joint function by 40%.
- Weight loss - even 10% helps. Every extra pound puts 4 pounds of pressure on your knee. Lose 10% of your body weight? You cut pain by nearly half. In one survey, 72% of people with OA reported major improvement after losing that much. It’s not about being thin. It’s about reducing load.
- Joint protection techniques. Learn how to stand, sit, and move without stressing your joints. Use your bigger muscles - hips and thighs - instead of your knees. Don’t kneel. Use a cane if needed. Take breaks. A certified physical therapist can teach you this in 6-8 sessions. It’s not fluff. It’s science.
- Education - the hidden key. The CDC’s 6-week self-management course cuts pain by 40% and improves function by 30%. Why? Because people learn what to do, what not to do, and how to talk to their doctors. Knowledge reduces fear. Fear makes you move less. Move less, and your joints get stiffer.
These four things aren’t optional extras. The American College of Rheumatology says you need at least three of them to manage OA effectively. Skip one, and you’re relying on luck.
What About Medications and Injections?
Painkillers? They help - but they’re not the solution.
NSAIDs like ibuprofen or naproxen reduce pain and inflammation. But 32% of people stop taking them because of stomach issues, high blood pressure, or kidney strain. And they don’t slow the disease. They just mask the pain - which can make you overuse your joint and cause more damage.
Acetaminophen? Works for mild pain, but studies show it’s no better than placebo for moderate-to-severe OA. And too much can hurt your liver.
So what works better?
Intra-articular corticosteroid injections. The OARSI guidelines now strongly recommend them for knee OA flare-ups. One injection can cut pain by 50% for up to 4 weeks. It’s not permanent. But it gives you a window - time to get moving, lose weight, start PT.
Tanezumab. The FDA approved this new nerve-blocking drug in June 2023. In trials, it reduced pain 35% more than NSAIDs. But it’s only for moderate-to-severe cases. And it’s not available everywhere yet.
Glucosamine and chondroitin? Most studies show they don’t work better than sugar pills. Save your money.
Stem cell or PRP injections? They’re trending. Over 380 clinical trials are running right now. But the evidence is still weak. Don’t pay $1,000+ for an unproven treatment.

The Hidden Costs - Beyond Pain
Osteoarthritis doesn’t just hurt. It changes your life.
68% of people with OA say pain keeps them from sleeping. 57% can’t climb stairs without help. 42% struggle with simple tasks like buttoning shirts. And it’s not just physical. The CDC says 43% of people with arthritis limit their work activities. That means lost income, lost confidence, lost independence.
And here’s the vicious cycle: you stop moving because it hurts. Then your muscles weaken. Your heart gets weaker. You gain weight. You get more pain. You move less. It spirals.
That’s why movement isn’t just about the joint. It’s about staying alive. Walking 30 minutes a day cuts your risk of heart disease, diabetes, and depression. It’s not a luxury. It’s survival.
Who’s Most at Risk - And Why
Women are more likely to get OA - 60% of cases. But men tend to have worse hip damage. Women get more knee and hand OA. Why? Hormones, joint structure, and body weight all play a role.
Age? Yes. But OA isn’t normal aging. You can be 70 and have no OA. You can be 40 and have severe OA.
Obesity? The biggest driver. 42% of U.S. adults are obese. That’s 100 million people at higher risk. Every extra pound multiplies the stress on your joints.
Occupation? Construction workers have a 37% higher risk. Dancers, plumbers, and professional musicians? Higher risk too. Repetitive motion. Heavy lifting. Kneeling. These aren’t just jobs - they’re joint stressors.
Genetics? Yes. If your mom had severe hand OA, you’re more likely to get it. But genes aren’t destiny. Lifestyle still controls the outcome.
What’s Coming Next
Researchers are working on blood tests that could detect OA years before symptoms show. Dr. Marc Hochberg predicts we’ll have them in five years. That means we could start treatment before the joint is damaged - not after.
The CDC’s "Active People, Healthy Nation" program is rolling out free community exercise classes in all 50 states. It’s not a drug. It’s a movement.
And the economic cost? It’s rising. OA costs the U.S. $140 billion a year. That’s more than diabetes. More than heart disease. And by 2040, 78 million Americans could have it - if nothing changes.
But here’s the truth: you don’t need to wait for a miracle drug. The tools are here. Exercise. Weight loss. Education. Joint protection. They’re not sexy. But they work. And they’re cheaper than pills, shots, or surgery.
Start today. Walk 10 minutes. Eat one less sugary snack. Call your local Arthritis Foundation office. Ask about their self-management course. Don’t wait until you can’t get out of bed. The joint degeneration won’t reverse - but your pain, your mobility, your life? That’s still yours to take back.
Is osteoarthritis the same as rheumatoid arthritis?
No. Osteoarthritis is caused by mechanical wear and biological breakdown of joint tissues. Rheumatoid arthritis is an autoimmune disease where your immune system attacks your joints, causing swelling, heat, and prolonged morning stiffness. OA pain gets worse with activity and improves with rest. RA pain often improves with movement and is worse in the morning.
Can you reverse osteoarthritis?
No, you can’t reverse the cartilage damage. But you can stop it from getting worse - and significantly reduce pain and improve function. Weight loss, exercise, physical therapy, and joint protection can make a big difference, even in advanced cases. Many people live active lives with OA by managing symptoms effectively.
Does walking make osteoarthritis worse?
No - if done correctly. Walking is one of the best exercises for OA. It strengthens muscles around the joint, improves circulation, and helps with weight control. Avoid high-impact surfaces and long distances at first. Start with short, flat walks and build up. Use supportive shoes. If walking causes sharp pain, stop and try swimming or cycling instead.
What’s the best pain reliever for osteoarthritis?
There’s no single best option. For mild pain, acetaminophen may help. For moderate pain and inflammation, NSAIDs like ibuprofen work - but they carry risks like stomach bleeding. Topical creams (like diclofenac gel) are safer and often just as effective for knees and hands. Injections of corticosteroids can give quick relief during flare-ups. Always talk to your doctor before starting any medication.
How long does it take to see results from exercise for osteoarthritis?
Most people start noticing less pain and better mobility after 4-6 weeks of consistent exercise. The Arthritis Foundation’s clinical trial showed 80% of participants had measurable improvement after 12 weeks. The key is consistency - not intensity. Doing 30-45 minutes of low-impact activity three times a week is more effective than one long, intense workout.
Can I still work with osteoarthritis?
Yes - but you may need adjustments. If your job involves standing, kneeling, or lifting, talk to your employer about ergonomic changes: sit-stand desks, padded mats, lighter tools, or flexible hours. The CDC reports 43% of people with arthritis limit work activities - but many of those limitations can be reduced with simple workplace modifications. You have rights under the ADA to request reasonable accommodations.

Jess Bevis
January 28, 2026 AT 02:11Walked 10 mins today. No pain. Who knew?
Rose Palmer
January 29, 2026 AT 03:14Thank you for this meticulously researched and clinically grounded overview. The distinction between osteoarthritis and rheumatoid arthritis is often muddled in public discourse, and your clarification of symptom patterns, inflammatory markers, and biomechanical causation is both accurate and urgently needed. The emphasis on non-pharmacological interventions aligns with current ACR guidelines and should be prioritized in primary care.
Howard Esakov
January 29, 2026 AT 05:10Bro. You just dropped the entire textbook on OA like it was a TikTok trend. 😎 I’m 38 and my knees sound like a bag of popcorn. But hey - at least I’m not one of those ‘glucosamine believers’ who thinks magic powders fix cartilage. 🤓
Kathy Scaman
January 29, 2026 AT 06:39I used to think it was just me being lazy. Turns out I just needed to stop ignoring the clicking. Started swimming twice a week. No more pain after work. Mind blown. 🙌
Mindee Coulter
January 30, 2026 AT 07:24Exercise works. I lost 12% of my weight and my knee stopped screaming. No magic. Just movement. And yes I still eat pizza but now I walk after
Timothy Davis
January 30, 2026 AT 10:59Let’s be real - 80% improvement from exercise? That’s cherry-picked data. Most people quit after two weeks. And you think people are gonna do 45 minutes three times a week when they’re already exhausted from work and kids? This is the kind of wellness propaganda that ignores systemic inequality. Not everyone has access to a pool, a gym, or the time. Stop pretending lifestyle fixes are universal.
Colin Pierce
January 30, 2026 AT 15:11Timothy’s got a point - it’s easy to say "just walk more" when you’ve got a safe neighborhood, a flexible job, and no chronic pain. I’ve been doing PT for 6 months. It helps, but I also need my steroid shot every 3 months. It’s not either/or. It’s both. And yeah, the CDC course? Life-changing. Free. Do it. But don’t shame people who need meds too.
Mark Alan
February 1, 2026 AT 10:11THEY’RE LYING TO YOU. 🚨 Big Pharma doesn’t want you walking - they want you buying pills. 🧪💉 The real cure? Cold therapy, magnesium, and not eating sugar. I’ve been pain-free for 2 years since I quit bread. OA is just inflammation. You’re not broken. You’re just fed wrong. 🇺🇸🔥
Ambrose Curtis
February 3, 2026 AT 07:03ok so i tried the walking thing and my knee felt like it was gonna explode on day 3. so i switched to cycling. 3x a week. now i can climb stairs without crying. also i started using a cane when i walk the dog. no shame. it’s like a mobility upgrade. also i stopped googling "can osteoarthritis be reversed" because now i know it’s about slowing it, not fixing it. big difference.
Jeffrey Carroll
February 5, 2026 AT 03:59The emphasis on education as a core pillar of OA management is profoundly correct. Knowledge empowers behavioral change, and behavioral change alters disease trajectory. The CDC’s self-management program is among the most underutilized public health tools available. I urge all clinicians to prescribe it as routinely as they prescribe NSAIDs.
Phil Davis
February 5, 2026 AT 17:54So… exercise, weight loss, education, and joint protection. Four things. Not five. Not ten. Four. And yet 90% of patients still walk out of the clinic with a prescription for ibuprofen. We’ve turned a biomechanical problem into a pharmaceutical one. And now we’re surprised it’s not working?
Sue Latham
February 6, 2026 AT 11:13glucosamine is literally just sugar with a fancy label. i spent $120 on that crap for 6 months. my knee still popped like a popcorn machine. now i just walk. and drink coffee. and ignore the clicking. it’s fine.
John Rose
February 7, 2026 AT 08:36I’m curious - has anyone here tried the new tanezumab? I’ve been reading about it but can’t find it locally. Is it worth asking my rheumatologist about? Or is it still too new and risky?