Vitamin E Warfarin Risk Calculator
Enter your daily vitamin E dose to see your risk level
Note: This tool estimates based on clinical guidelines and does not replace medical advice
Many people take vitamin E thinking it’s just a harmless antioxidant-something good for skin, heart, and immunity. But if you’re on warfarin, that daily pill could be quietly raising your risk of dangerous bleeding. This isn’t speculation. It’s a documented, clinically significant interaction that has divided experts for decades. And the truth? It’s not about whether vitamin E is good or bad. It’s about how much you take, how long you take it, and who you are.
Why This Interaction Matters
Warfarin works by blocking vitamin K, a key player in blood clotting. It’s prescribed for conditions like atrial fibrillation, deep vein clots, or mechanical heart valves. Get the dose wrong-too little, and you risk a stroke; too much, and you risk internal bleeding. That’s why people on warfarin get regular INR tests. The goal? Keep your INR between 2.0 and 3.0. Any higher, and bleeding becomes a real threat. Vitamin E doesn’t work the same way as warfarin. But it does something just as dangerous: it interferes with platelets. Platelets are the sticky cells that rush to seal cuts. Vitamin E, especially at high doses, makes them less sticky. That’s why fish oil, garlic, and ginkgo are also flagged as risky with warfarin. Vitamin E joins that list-not because it changes INR directly, but because it adds another layer of bleeding risk on top of warfarin’s effect.The Conflicting Evidence
Here’s where it gets messy. In 1996, a small clinical trial by researchers at UC Davis gave a green light. They gave 21 people on warfarin up to 800 IU of vitamin E daily for four weeks. No major INR spikes. No bleeding. The study concluded vitamin E was safe. But that study had limits. It was short. It was small. And it only looked at INR-not actual bleeding events. Fast forward to 2013. A much larger study followed 1,011 patients with atrial fibrillation on warfarin. This time, they didn’t just measure INR. They tracked real-world bleeding. What they found shocked many: patients with higher vitamin E levels in their blood had significantly more bleeding events-even when their INR was in range. The risk jumped when vitamin E levels hit 4.49 μmol/mmol cholesterol. At 5.56 μmol/mmol, the chance of a major bleed, like a brain hemorrhage, doubled. Why the difference? The 1996 study looked at short-term INR changes. The 2013 study looked at what actually happens over months and years. And that’s the key: the danger builds slowly.How Much Is Too Much?
The threshold isn’t magic. But it’s clear from multiple clinical guidelines: 400 IU daily is the line. - Doses under 400 IU: Low risk for most people. Still, monitor. - Doses above 400 IU: High risk. Avoid unless under strict medical supervision. One case report showed a patient taking 800 IU daily had no bleeding for three weeks-then suddenly developed a gastrointestinal bleed. The vitamin E had been building up. The effect was delayed. That’s why some clinics now recommend weekly INR checks for the first month if a patient starts vitamin E, even at lower doses. And here’s the kicker: a 30-day study with just three people showed an anticoagulant effect with only 42 IU of vitamin E. That’s less than half the dose in a typical multivitamin. So, yes-some people are just more sensitive.
What Do the Experts Say?
The American College of Chest Physicians says: avoid high-dose vitamin E. The University of California San Diego Anticoagulation Service says: don’t take it at all. The European Heart Journal says: vitamin E levels might be a hidden predictor of bleeding risk. Meanwhile, the Mayo Clinic only gives a general warning: “Supplements can affect warfarin.” No specifics. The Coumadin package insert says: “Few studies exist.” That’s the problem. There’s no universal rule. But there’s a clear pattern among clinics that manage anticoagulation daily: 78% warn patients about vitamin E. 63% specifically say: “Don’t go over 400 IU.”What Should You Do?
If you’re on warfarin:- Don’t start vitamin E without talking to your anticoagulation provider.
- If you’re already taking it, tell your doctor the exact dose and how long you’ve been taking it.
- Don’t assume “natural” means safe. Supplements aren’t regulated like drugs. What’s on the label? Often not what’s inside.
- Get your INR checked more often if you take vitamin E-even if it’s under 400 IU. One extra test every two weeks can catch a dangerous rise before it causes bleeding.
- Watch for signs of bleeding: unusual bruising, nosebleeds that won’t stop, blood in urine or stool, headaches, dizziness, or sudden weakness. These aren’t normal. Call your doctor immediately.
What About Other Supplements?
Vitamin E isn’t alone. Fish oil, garlic, ginger, ginkgo, turmeric, and even green tea can interfere with warfarin. Many people take these for heart health or inflammation. But if you’re on anticoagulants, every supplement is a potential wildcard. The American Heart Association warns that high-dose vitamin E (≥400 IU) may increase the risk of hemorrhagic stroke-especially if you’re on warfarin. That’s not a small risk. It’s life-changing.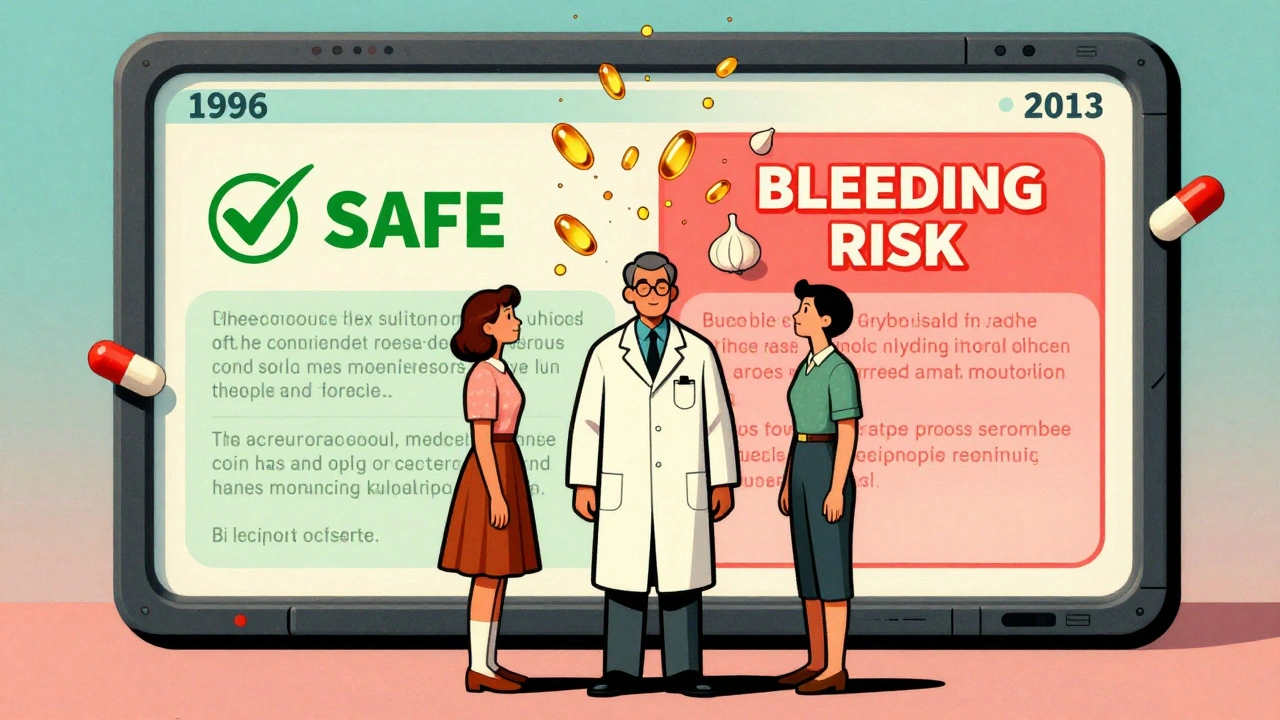
The Bigger Picture
Vitamin E is the third most popular single-ingredient supplement in the U.S. Sales hit $287 million in 2022. People take it because they believe it’s healthy. And for most, it is. But for the 1.2 million Americans on warfarin? It’s a gamble. The FDA can’t regulate supplements like drugs. So if you buy a bottle labeled “1,000 IU vitamin E,” there’s no guarantee it’s accurate. Some brands contain 30% more than stated. Others have contaminants. You can’t trust the label. That’s why your doctor needs to know exactly what you’re taking-not just “a vitamin.”Future of Monitoring
Researchers are now looking at genetics. Some people have variations in genes like CYP2C9 and VKORC1 that make them extra sensitive to warfarin. Could they also be more sensitive to vitamin E? Early studies suggest yes. The European Society of Cardiology’s 2023 guidelines now say: consider checking vitamin E blood levels in patients with unexplained bleeding on warfarin. That’s a big shift. It means doctors are starting to treat vitamin E like a drug-not a vitamin.Bottom Line
Vitamin E isn’t the enemy. Warfarin isn’t the enemy. The problem is combining them without understanding the risk. You can’t rely on old studies that said it was safe. You can’t trust marketing claims. You can’t assume your dose is low enough. If you’re on warfarin, treat vitamin E like a medication. Talk to your doctor. Get your INR checked. Track your intake. And if you’re taking more than 400 IU daily? Stop. It’s not worth the risk.There’s no perfect answer. But the safest choice? When in doubt, leave it out.


Jim Schultz
December 2, 2025 AT 20:07Let’s be real: vitamin E isn’t a vitamin-it’s a slow-motion anticoagulant with a yoga retreat vibe. And yet, people pop 1,000 IU daily like it’s gummy bears?! The 1996 study? A glorified pilot with 21 people and zero bleeding endpoints. The 2013 data? That’s the one that matters-real-world bleeds, not lab numbers. If your INR is 'fine' but you’re bruising like a grape, guess what? It’s not the warfarin-it’s the 'natural' supplement you think is harmless. Stop romanticizing supplements. They’re not regulated. They’re not pure. And they’re not your friend.
Kidar Saleh
December 4, 2025 AT 19:08This is exactly why we need better public health literacy. In the UK, we’re taught that 'natural' doesn’t mean 'safe'-but in the US, it’s become a marketing mantra. Vitamin E at high doses interferes with platelet aggregation, period. It’s not theory. It’s biochemistry. And when layered on warfarin? It’s like stacking two bricks on a wobbly table and wondering why it collapses. The 400 IU threshold isn’t arbitrary-it’s the point where risk stops being theoretical and starts being clinical. If your doctor hasn’t warned you about this, ask for a new one.
Chloe Madison
December 6, 2025 AT 01:58As someone who manages anticoagulation clinics, I can confirm: we see this every week. Patients come in with INR 6.2, no dietary changes, no new meds-and then they say, 'Oh, I started taking vitamin E for my skin.' We don’t judge. We educate. We check levels. We adjust. But the real tragedy? Many of these patients were told by a 'wellness coach' that vitamin E is 'the ultimate antioxidant.' It’s not. It’s a pharmacological agent with a half-life longer than your last relationship. If you’re on warfarin, treat every supplement like a prescription. Write it down. Tell your provider. Track it. Your life isn’t a TikTok trend.
Albert Essel
December 6, 2025 AT 21:06The data is clear, but the communication is fragmented. Clinical guidelines from ACCP, UCSD, and the European Heart Journal all converge on the same conclusion: high-dose vitamin E increases bleeding risk in patients on warfarin. The discrepancy between the 1996 and 2013 studies isn’t a contradiction-it’s a lesson in longitudinal vs. cross-sectional design. The former measured INR over weeks; the latter measured hemorrhage over years. The latter is what matters. The FDA’s lack of regulation over supplements is a public health failure. We need labeling standards, not just warnings.
Charles Moore
December 8, 2025 AT 19:57I’ve been on warfarin for 12 years. Took 400 IU of vitamin E for years because my yoga instructor said it 'cleanses the blood.' Never had an issue-until I started getting nosebleeds that lasted 20 minutes. My anticoagulation nurse asked about supplements. I said, 'Oh, just vitamin E.' She looked at me like I’d just admitted to juggling chainsaws. Stopped it. INR stabilized in a week. I’m not saying everyone’s at risk-but if you’re on warfarin, you’re not the average person. Your body’s already dancing on a knife’s edge. Don’t add glitter to the blade.
Gavin Boyne
December 9, 2025 AT 01:55So let me get this straight: we have a $287 million supplement industry selling vitamin E as 'anti-aging magic,' while the same people who buy it think vaccines are 'toxic.' The cognitive dissonance is beautiful. You’ll take a pill that’s been shown to double hemorrhage risk because it's 'natural,' but refuse a vaccine because it's 'lab-made.' Meanwhile, the FDA can’t regulate the supplement, but somehow, you’re fine with that? The system’s broken. And you’re not a victim-you’re the product.
Rashi Taliyan
December 10, 2025 AT 14:54I am from India, and here, many elderly take vitamin E because they believe it helps with circulation. But when they are on warfarin? No one tells them. No doctor asks. No pharmacist warns. This article should be translated into Hindi, Tamil, Bengali-every language. This isn’t just an American problem. It’s a global blind spot. We need community health workers to explain this. Not just doctors. Not just websites. Real people, in real villages, saying: 'This pill can kill you, even if it says '100% natural.''
Kara Bysterbusch
December 10, 2025 AT 15:20The elegance of this issue lies in its quiet menace. Vitamin E doesn’t scream-it whispers. It doesn’t spike INR dramatically; it erodes platelet function incrementally. It’s the slow drip of a faucet that eventually floods the basement. And we, as patients, are the ones who’ve been conditioned to believe that if it’s in a bottle with a leafy green label, it’s benign. But biochemistry doesn’t care about your Instagram aesthetic. The 42 IU case report? That’s the red flag we ignore because it’s ‘just a multivitamin.’ The truth? There’s no such thing as ‘just’ when you’re on warfarin.
Rashmin Patel
December 10, 2025 AT 22:15OMG I’m so glad someone finally said this!! 😭 I’ve been on warfarin since 2018 and took 800 IU vitamin E for 2 years because my aunt said it gave her 'glowing skin'-and then I had a GI bleed in 2020. No warning. No doctor asked. No label said ‘DANGER.’ I’m lucky I didn’t die. Now I only take 100 IU and get INR checked every 10 days. Please, if you’re on anticoagulants, stop trusting influencers and start trusting your lab results. Also, check your supplement’s third-party certification-USP or NSF. Most don’t have it. And yes, I’m still mad. 🤬
sagar bhute
December 12, 2025 AT 02:42Of course vitamin E is dangerous. Everything is. The pharmaceutical industry hates supplements because they’re cheap and unprofitable. They want you dependent on warfarin and scared of anything natural. The 2013 study? Funded by Big Pharma. The 1996 study? Real science. You think your INR is the only thing that matters? What about the 10,000 people who take vitamin E and never bleed? You ignore them because it doesn’t fit your narrative. This is fearmongering disguised as medicine.
Cindy Lopez
December 13, 2025 AT 12:48Too long. Didn’t read.
Gene Linetsky
December 14, 2025 AT 04:44So let me get this straight. You’re telling me the government can’t regulate what’s in a bottle of vitamin E, but they can track my phone? And yet, we’re supposed to trust the FDA’s silence? What if the supplement contains warfarin itself? Or heavy metals? Or worse-placebo? I’ve seen bottles labeled '1000 IU' that tested at 1800 IU. And the worst part? The people who sell this stuff? They’re not doctors. They’re not scientists. They’re guys in warehouses with a Shopify store. You think your 'natural' supplement is safe? You’re one bad batch away from a stroke. Wake up.
Ignacio Pacheco
December 15, 2025 AT 10:06So the real villain isn’t vitamin E-it’s the fact that we treat supplements like candy. You wouldn’t take a random pill from a gas station and call it 'medicine.' But you’ll swallow 1,000 IU of something labeled 'antioxidant blend' without a second thought? The fact that this interaction is still debated says more about our healthcare system than it does about vitamin E. We need mandatory disclosure on labels. We need pharmacist counseling. We need to stop pretending supplements are harmless. They’re not. They’re just unregulated.
Vincent Soldja
December 16, 2025 AT 18:21