Vaginal Burning Symptom Checker
Select your symptoms and click "Analyze Symptoms" to get personalized insights
Key Takeaways
- High blood sugar can create an environment that favors yeast overgrowth, a common cause of vaginal burning.
- Poor circulation and nerve damage from diabetes may heighten irritation and reduce healing.
- A proper diagnosis often combines blood‑glucose tests with a simple vaginal swab.
- Keeping glucose stable, practicing good hygiene, and treating infections quickly can ease symptoms.
- If burning persists despite treatment, talk to a healthcare provider-there could be another underlying issue.
When vaginal burning refers to a painful, tingling or stinging sensation inside the vagina meets diabetes mellitus a chronic condition where the body struggles to regulate blood sugar, many women notice a puzzling link. The connection isn’t magic-it’s rooted in how high glucose levels change the vaginal ecosystem, affect nerves, and alter blood flow. Below we break down the science in plain language and give you a roadmap for relief.
What Is Vaginal Burning?
Vaginal burning feels like a low‑grade fire or an electric shock that can flare up during urination, after sex, or even at rest. The sensation often comes with itching, redness, or a watery discharge. While the symptom itself isn’t a disease, it signals that something inside the vagina is out of balance. Common culprits include infections, hormonal shifts, moisture‑locked clothing, and, as we’ll see, uncontrolled diabetes.
Diabetes in a Nutshell
Diabetes mellitus splits into two main types: Type1 an autoimmune condition where the pancreas produces little to no insulin and Type2 characterized by insulin resistance and often linked to weight and lifestyle factors. Both types raise blood glucose the concentration of sugar circulating in the bloodstream and, over time, can damage nerves, blood vessels, and the immune system. Those changes set the stage for vaginal irritation.
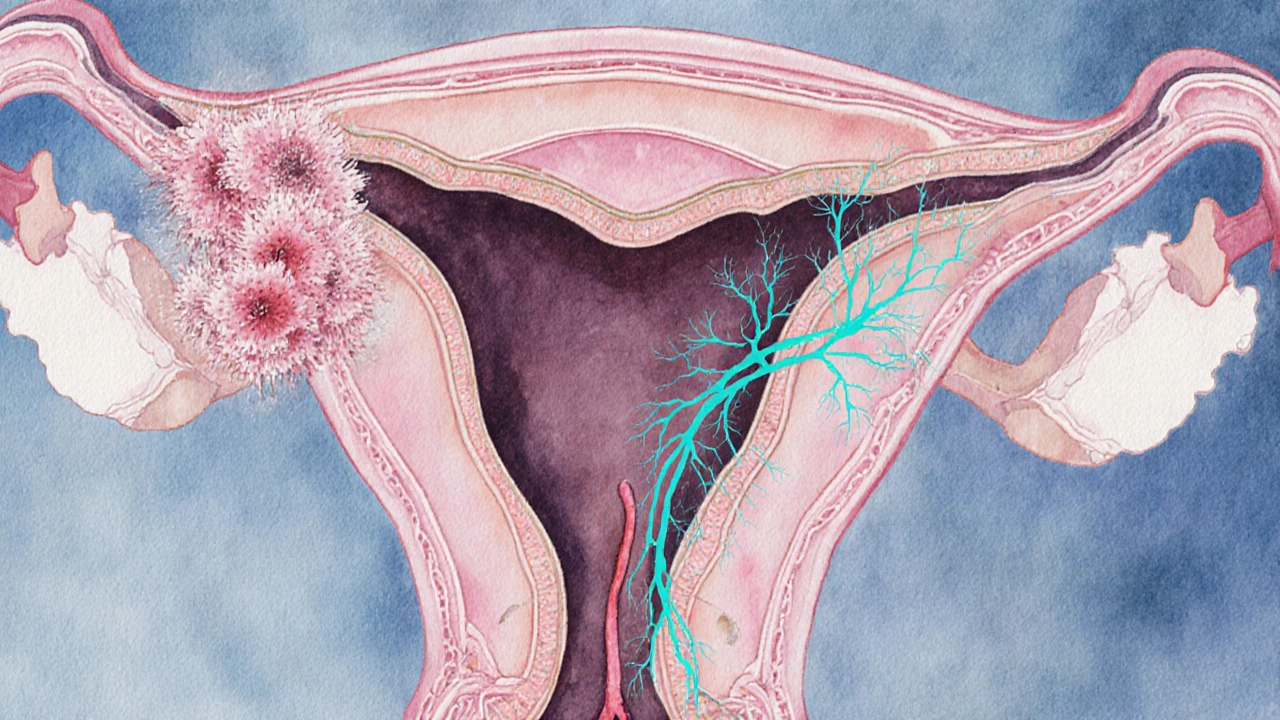
How Diabetes Triggers Vaginal Burning
Three biological pathways explain why diabetic women report more burning:
- Yeast overgrowth - Elevated glucose spills into vaginal fluids, feeding Candida albicans the fungus that causes most yeast infections. A thriving yeast colony produces acids that irritate the lining, leading to that familiar sting.
- Nerve damage (diabetic neuropathy) - Chronic high sugar damages peripheral nerves, including those supplying the pelvic region. Damaged nerves transmit pain signals more intensely, turning a mild irritation into a burning sensation.
- Reduced blood flow - Diabetes thickens blood vessels, limiting oxygen and nutrient delivery to vaginal tissue. Poor circulation hampers healing and makes the mucosa more sensitive to everyday friction.
On top of these, hormonal fluctuations tied to insulin resistance can thin the vaginal walls, adding another layer of vulnerability.
Spotting the Symptoms and Deciding When to See a Doctor
If you notice any of the following, it’s time to schedule a visit:
- A burning feeling that lasts more than a few days.
- Thick, white, cottage‑cheese‑like discharge (a sign of yeast infection).
- Clear, cloudy, or foul‑smelling urine that accompanies the sting (possible urinary tract infection).
- Redness, swelling, or bleeding without an obvious cause.
Because the same symptom can stem from different problems, a professional evaluation prevents mis‑treatment.
How Doctors Diagnose the Issue
Diagnosis usually combines two streams:
- Blood tests - Your provider will check fasting glucose and HbA1c the percentage of hemoglobin bound to sugar, reflecting average glucose over 2‑3 months. Poor control points to a higher infection risk.
- Vaginal examination - A quick swab assesses pH, looks for yeast cells under a microscope, and may culture bacteria to rule out a urinary tract infection or bacterial vaginosis.
In uncertain cases, an ultrasound can check for structural issues, and a nerve‑conduction test can confirm neuropathy.
Managing Vaginal Burning When You Have Diabetes
The cure‑all is good glucose control. Here’s a step‑by‑step plan that tackles both the root cause and the symptoms:
- Stabilize blood sugar - Aim for fasting glucose between 80‑130mg/dL and an HbA1c below 7% (or your doctor’s target). Use medication, diet, and regular exercise.
- Treat the infection - If a yeast infection is confirmed, an over‑the‑counter azole cream (e.g., clotrimazole) for 7days works for most cases. Recurrent infections may need a short oral antifungal prescribed by a clinician.
- Address neuropathy - Medications such as gabapentin or duloxetine can dull nerve pain. Physical therapy focused on pelvic floor relaxation also helps.
- Boost vaginal health - Switch to cotton underwear, avoid scented soaps, and rinse the area with plain water after intercourse or swimming.
- Consider probiotics - LactobacillusrhamnosusGR‑1 andLactobacillusreuteriRC‑14 have shown promise in maintaining a healthy vaginal flora, especially when glucose is high.
Track progress in a journal: note glucose readings, symptom intensity, and any triggers you spot. Patterns will guide you and your doctor toward fine‑tuning the plan.
Prevention Tips for the Long Term
Preventing the next flare‑up is easier than treating it after it starts. Try these habits:
- Keep glucose levels steady - small, balanced meals every 3‑4hours reduce spikes.
- Stay hydrated - drinking plenty of water helps flush the urinary tract and keeps vaginal tissue moist but not overly wet.
- Wear breathable fabrics - cotton and moisture‑wicking sportswear let the area breathe.
- Avoid irritants - ditch douches, scented wipes, and tight synthetic pantyhose.
- Schedule regular check‑ups - annual gynecological exams catch early changes before they become painful.
Comparison of Common Causes of Vaginal Burning
| Cause | Typical Symptoms | Key Diagnostic Test | First‑line Treatment |
|---|---|---|---|
| Diabetes‑related yeast infection | Burning, itching, thick white discharge | Vaginal swab showing Candida | Topical azole antifungal + glucose control |
| Urinary tract infection | Burning on urination, cloudy urine, urgency | Urine culture | Oral antibiotics (e.g., trimethoprim‑sulfamethoxazole) |
| Bacterial vaginosis | Fishy odor, thin gray discharge, mild irritation | Vaginal pH > 4.5, clue cells on microscopy | Metronidazole gel or oral tablet |
| Hormonal imbalance (menopause, contraceptives) | Dryness, mild burning, occasional spotting | Serum estrogen/progesterone levels | Local estrogen cream or hormonal adjustment |
| Irritants (soaps, tight clothing) | Localized redness, burning after exposure | Clinical exam, patient history | Avoid trigger, use barrier creams |

Frequently Asked Questions
Can tight blood sugar control eliminate vaginal burning?
Good control reduces the sugar that feeds yeast and eases nerve irritation, so many women see a big improvement. However, if an infection is already present, you’ll still need targeted treatment.
How fast does a yeast infection clear up with treatment?
Over‑the‑counter creams usually relieve symptoms within 3‑5 days, though the full course is 7 days to prevent recurrence.
Is vaginal burning ever a sign of something more serious?
Yes. Persistent burning with no clear infection could hint at diabetic neuropathy, autoimmune conditions, or even early signs of cancer. Persistent or worsening symptoms warrant a thorough evaluation.
Do probiotics really help prevent yeast infections?
Studies show that daily oral probiotics containing Lactobacillus strains can maintain a healthy vaginal pH and lower recurrence rates, especially when blood sugar is well‑managed.
Can I use the same antifungal cream while pregnant?
Most topical azoles are considered safe in pregnancy, but it’s best to confirm with your obstetrician before starting any medication.

michael santoso
October 1, 2025 AT 17:38While the article does a decent job of summarizing the pathophysiology, it glosses over the nuanced interplay between hyperglycemia‑induced immunosuppression and mucosal barrier integrity. A more rigorous discussion of the microbiome shifts would have elevated the piece from a lay‑summary to a scholarly review. Moreover, the lack of citation to recent longitudinal studies on diabetic neuropathy is a glaring omission.
M2lifestyle Prem nagar
October 1, 2025 AT 19:52Staying on top of glucose can seriously cut down those annoying burning episodes.
Karen Ballard
October 1, 2025 AT 22:05Great rundown! 👍 The link between high sugar and yeast overgrowth is spot on. 🌟 Keep the practical tips coming.
Gina Lola
October 2, 2025 AT 00:18Just to throw some jargon into the mix: the dysbiosis you mention is essentially a shift in the vaginal microbiota towards a higher Candida albidus quotient. That’s why you feel the sting during micturition.
Leah Hawthorne
October 2, 2025 AT 02:32I appreciate the balanced tone here; it acknowledges both infection and neuropathy without sounding alarmist. Keeping the advice practical-like cotton underwear and glucose monitoring-makes it actionable.
Kevin Huston
October 2, 2025 AT 04:45Honestly, this piece feels like it was cobbled together by a committee terrified of offending anyone. The language is as bland as boiled chicken, and the recommendations are a generic checklist you’d find on any discount health blog.
Amanda Hamlet
October 2, 2025 AT 06:58i think u missed the point whre the real issue is that diabetics get low self esteem because they cant even stop the burng. its not just a simple infection its a whole systemic probelm .
Nolan Jones
October 2, 2025 AT 09:12From a clinical standpoint, the three mechanisms listed-yeast overgrowth, neuropathy, and vascular insufficiency-cover the major bases. If you’re dealing with recurrent episodes, a mycological culture is a good next step. Also, consider a referral to a podiatrist if you suspect peripheral neuropathy.
Jada Singleton
October 2, 2025 AT 11:25Reading this feels like a thinly veiled attempt to normalize chronic discomfort. If the burning persists beyond a week, you’re *not* just being dramatic; you’re likely confronting an underlying pathology that deserves scrutiny.
Emily Rossiter
October 2, 2025 AT 13:38Valid point about persistence. It’s important to listen to your body and seek professional help when home remedies don’t bring relief. You deserve care that addresses both symptoms and root causes.
Renee van Baar
October 2, 2025 AT 15:52First, let’s acknowledge that the emotional toll of chronic vaginal burning can be substantial, especially when paired with the stress of managing diabetes.
Second, the article correctly identifies hyperglycemia as a catalyst for Candida overgrowth, but it could expand on how fluctuating glucose spikes create a permissive environment for other opportunistic organisms as well.
Third, the discussion on neuropathy is useful; however, many patients confuse peripheral neuropathic pain with superficial burning caused by irritation, leading to delayed treatment.
Fourth, the recommendation to keep a symptom journal is gold-tracking blood glucose, diet, and symptom intensity can reveal patterns that inform both endocrinologists and gynecologists.
Fifth, while cotton underwear is a staple suggestion, the article might also mention the role of breathable athletic fabrics for active individuals.
Sixth, hydration is vital, not just for urinary health but also for maintaining mucosal moisture, which can mitigate dryness‑related burning.
Seventh, the piece briefly mentions probiotics; recent trials show that daily Lactobacillus rhamnosus GR‑1 can reduce recurrence rates in diabetic women by up to 30 %.
Eighth, the table summarizing causes is helpful, but a column on typical treatment duration would aid readers in setting realistic expectations.
Ninth, for those with confirmed yeast infections, a 7‑day azole regimen is standard, yet refractory cases may need a short course of oral fluconazole.
Tenth, the article could address the psychological impact, encouraging patients to discuss sexual health concerns with their partners.
Eleventh, a note on menopause‑related estrogen decline intersecting with diabetes would broaden the audience.
Twelfth, the suggestion to schedule annual gynecological exams is sound; early detection of atypical lesions can prevent progression to more serious conditions.
Thirteenth, consider the role of tight glycemic control not only in reducing infection risk but also in improving overall nerve health.
Fourteenth, for patients experiencing burning on urination, a urinalysis is essential to rule out concurrent UTIs.
Fifteenth, the article wisely advises seeking professional evaluation if symptoms persist, which cannot be overstated.
Sixteenth, overall, the guide is a solid starting point, yet incorporating these additional nuances would transform it from a good overview to a comprehensive resource.
Mithun Paul
October 2, 2025 AT 18:05While the preceding discourse is thorough, it suffers from a lack of citation to primary literature, thereby diminishing its evidentiary weight.
Sandy Martin
October 2, 2025 AT 20:18I’ve been there-persistent burning is frightening, and the uncertainty can feel isolating. Remember you’re not alone, and there are clinicians who specialize in diabetic gynecologic health.
Steve Smilie
October 2, 2025 AT 22:32One might question whether the emphasis on lifestyle modifications is a subtle attempt to shift responsibility onto patients rather than addressing systemic healthcare gaps.
Josie McManus
October 3, 2025 AT 00:45It’s crucial to advocate for yourself; if your doctor dismisses the burning as "just a symptom," ask for a referral to an endocrinology‑gynecology specialist who understands the interplay.
Heather Kennedy
October 3, 2025 AT 02:58From a clinical informatics perspective, integrating continuous glucose monitoring data with symptom logs could enable predictive analytics for flare‑ups.
Janice Rodrigiez
October 3, 2025 AT 05:12Quick tip: over‑the‑counter azole creams are effective when used for the full 7‑day course-don’t stop early.
Roger Cardoso
October 3, 2025 AT 07:25Honestly, the whole "stay hydrated" mantra is a marketing ploy; real improvement comes from addressing the underlying insulin resistance, not drinking extra water.