Therapeutic Substitution: When Swapping Medications Makes Sense
When your doctor switches your brand-name drug for a cheaper version that does the same job, that’s therapeutic substitution, the practice of replacing one medication with another from the same class that has similar clinical effects. Also known as drug substitution, it’s not just about cost—it’s about keeping treatment effective while reducing financial strain on patients and healthcare systems. This isn’t random. It’s a deliberate, evidence-based move backed by clinical guidelines and real-world outcomes.
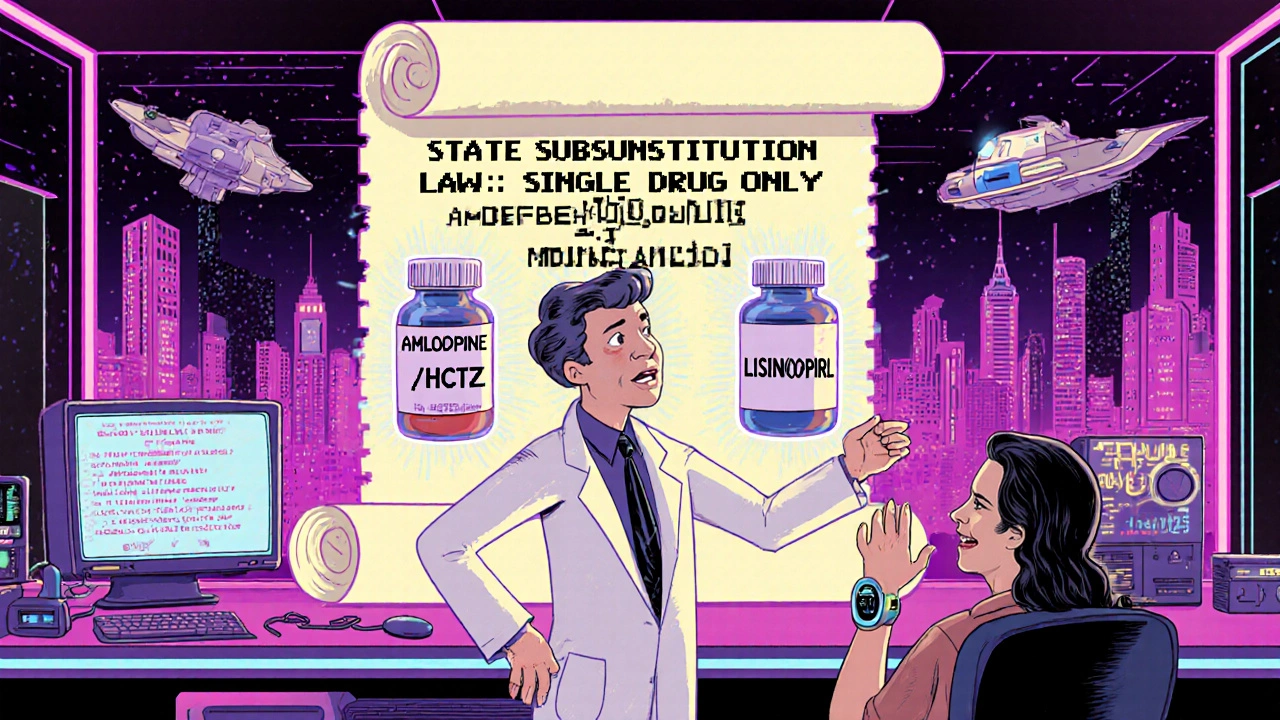
Therapeutic substitution often involves generic drugs, medications with the same active ingredient as brand-name versions but sold under their chemical name. Also known as non-brand medications, they’re the most common form of substitution you’ll see—like swapping Lipitor for atorvastatin or Prilosec for omeprazole. But it doesn’t stop there. Sometimes, a doctor will switch you from one brand to another brand in the same class—like swapping lisinopril for losartan for blood pressure. That’s still therapeutic substitution, and it’s guided by data on effectiveness, side effects, and how your body responds. These decisions rely on drug alternatives, medications with similar mechanisms of action that can be used interchangeably under clinical supervision. Also known as equivalent therapies, they’re the backbone of smart prescribing. Think of it like choosing between two different brands of pain reliever: both have ibuprofen, so one works just as well as the other.
But not all substitutions are safe. Some drugs have narrow therapeutic windows—tiny differences in dosage or formulation can cause big problems. That’s why medication switching, the process of changing from one drug to another for therapeutic reasons. Also known as drug interchange, it requires careful monitoring. For example, switching from one antiepileptic to another isn’t like swapping painkillers. One study showed that even small changes in generic levothyroxine formulations can raise TSH levels in sensitive patients. That’s why your doctor might avoid substitution if you’re on thyroid meds, blood thinners, or seizure drugs. It’s not about distrust—it’s about precision.
Therapeutic substitution isn’t just a pharmacy trick. It’s part of pharmacotherapy, the use of drugs to treat disease, tailored to individual needs and outcomes. Also known as drug therapy, it’s the foundation of modern medicine. Every post in this collection ties back to this idea: when can you safely switch? When should you hold off? And how do you know if the swap is working? You’ll find real comparisons—like Aldactone vs. its alternatives, minoxidil vs. finasteride, or desloratadine vs. loratadine. These aren’t theoretical debates. They’re decisions real people make every day. Some save money. Some reduce side effects. Some just work better for your body. This page doesn’t tell you what to do. It gives you the facts so you can ask the right questions.