Tacrolimus Neurotoxicity Risk Calculator
Tacrolimus Risk Assessment Tool
This tool helps you understand your risk of neurotoxicity based on your tacrolimus blood level and transplant type. Remember: symptoms can occur even when levels are in the 'safe' range.
Your Risk Assessment
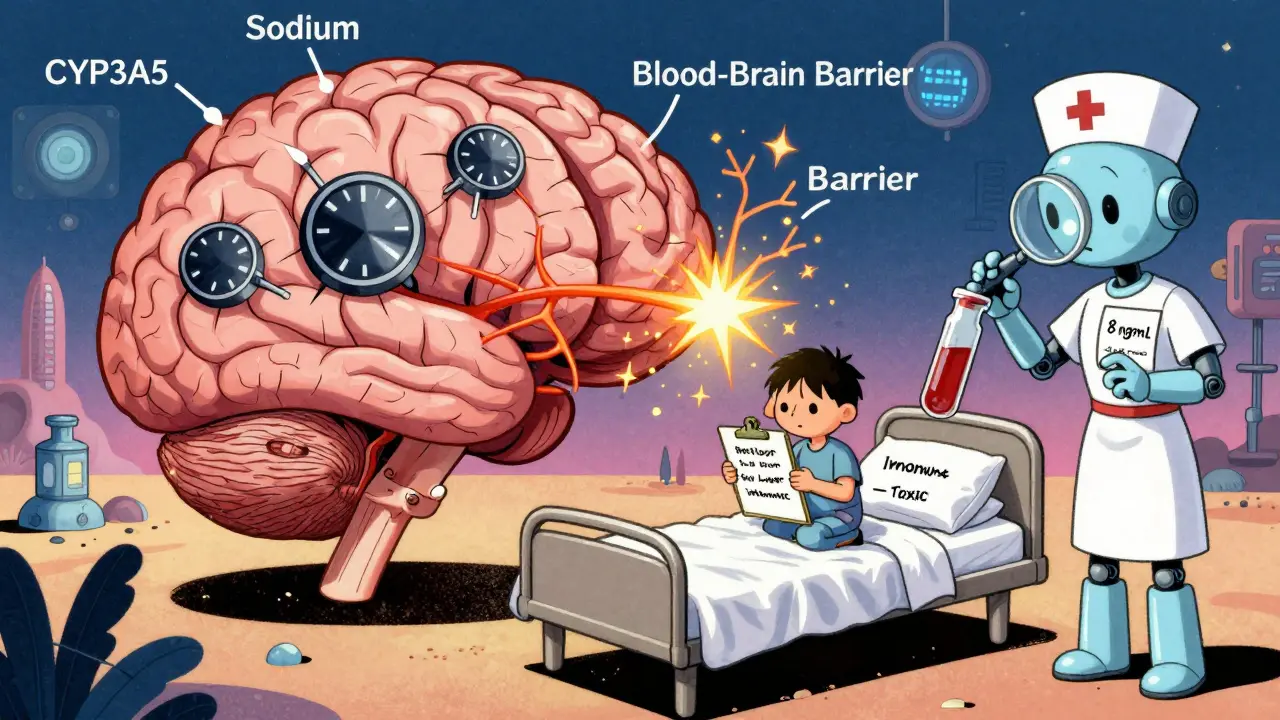
Important: This tool shows your risk based on blood levels only. Neurotoxicity can occur even at levels considered "safe" due to individual differences in blood-brain barrier permeability and genetics.
When you’ve just had a transplant, the relief of a functioning organ is real. But for many, that relief is quickly shadowed by a shaking hand, a pounding headache, or trouble sleeping. These aren’t just bad days-they’re signs of tacrolimus neurotoxicity, a common and often misunderstood side effect of one of the most widely used immunosuppressants in transplant care.
What Is Tacrolimus, and Why Is It So Common?
Tacrolimus is a powerful drug that keeps your body from rejecting a new kidney, liver, heart, or lung. It works by blocking calcineurin, a protein that activates immune cells. Without it, your immune system would attack the transplanted organ like an invader. Since its FDA approval in 1994, it’s become the go-to choice for most transplant centers because it cuts rejection rates by 20-30% compared to older drugs like cyclosporine. But there’s a catch. While it protects your new organ, it can also mess with your brain and nerves. About 1 in 3 transplant patients on tacrolimus will develop some form of neurotoxicity. And here’s the thing: it doesn’t always happen when blood levels are too high. Even people with levels in the "safe" range can get symptoms.The Most Common Symptoms: Tremor and Headache
If you’re on tacrolimus and notice something off, start with the two most frequent signs: tremor and headache. Tremor shows up in 65-75% of people who experience neurotoxicity. It’s not just a slight shake. For many, it’s enough to make holding a cup, writing a note, or buttoning a shirt impossible. One patient on the American Transplant Foundation forum described it as "my fingers moving like they had a mind of their own." It often starts within the first few weeks after transplant, even when blood levels are perfectly normal-like 7.2 ng/mL, which is well within the target range. Headache is the second most common symptom, affecting 45-55% of patients. These aren’t typical tension headaches. They’re often described as crushing, constant, and unresponsive to regular painkillers. One liver transplant recipient on Reddit said, "I took ibuprofen, Tylenol, even triptans-nothing touched it. Only when they switched me to cyclosporine did it finally go away." These symptoms don’t just annoy you-they impact your life. A 2022 survey of over 1,200 transplant patients found that 42% said their tremor made daily tasks so hard they had to stop working or cut back on activities. Headaches kept others from sleeping, concentrating, or even leaving the house.Other Neurological Signs You Shouldn’t Ignore
Tremor and headache are the tip of the iceberg. Other symptoms can sneak in quietly:- Insomnia or trouble sleeping (30-40%)
- Paresthesia-a tingling or numbness in hands or feet (30-40%)
- Weakness or fatigue that doesn’t go away (15-20%)
- Somnolence-feeling drowsy even after a full night’s sleep (10-15%)
- Confusion, agitation, or delirium (8-12%)
- Ataxia-trouble walking, stumbling, or losing balance (5-8%)
What Are the Right Blood Levels? And Why Do Levels Lie
Doctors measure tacrolimus levels in your blood to make sure you’re getting enough to prevent rejection but not so much that you get toxic. The standard ranges look like this:- Kidney transplant: 5-15 ng/mL
- Liver transplant: 5-10 ng/mL
- Heart transplant: 5-10 ng/mL
Who’s Most at Risk?
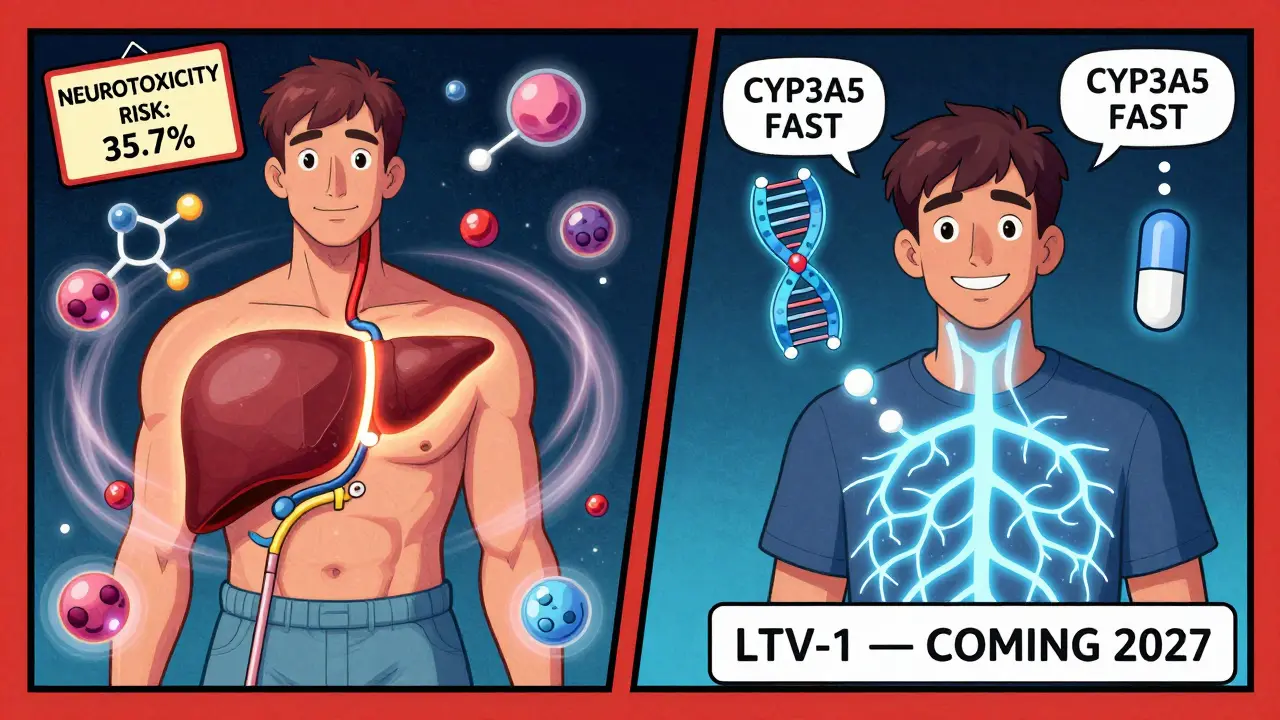
Not all transplant patients face the same risk. Liver recipients have the highest rate-35.7%-followed by kidney (22.4%), lung (18.9%), and heart (15.2%). Why? The liver is the main organ that breaks down tacrolimus. When it’s transplanted, the new liver might process the drug differently than the old one did. That can cause wild swings in blood levels, especially in the first weeks. Other risk factors:- Low sodium levels (hyponatremia)-found in 7 out of 12 studies as a trigger
- High blood pressure
- Using other drugs that stress the nervous system: antibiotics like linezolid, sedatives like midazolam, or antipsychotics like risperidone
- Older age and pre-existing neurological conditions
What Do You Do When Symptoms Show Up?
The first step is recognizing it’s not "just stress" or "post-op fatigue." Too often, patients wait weeks before their team connects the dots. One survey found 55% of patients said it took their doctors 2-3 weeks to realize the symptoms were from tacrolimus. If you notice tremor, headache, or confusion:- Don’t wait. Tell your transplant team immediately.
- Ask for a tacrolimus blood level check-and request it be done at the same time of day as your last test for consistency.
- Request a sodium level test. Low sodium is a hidden trigger.
- Review all other medications. Are you on any new antibiotics, pain meds, or sleep aids?
- Reduce the tacrolimus dose by 10-20%. Many patients see improvement in 3-7 days.
- Switch to cyclosporine. It’s less effective at preventing rejection (20-30% higher risk), but it causes neurotoxicity half as often.
What’s Next? The Future of Safer Immunosuppression
The truth is, we still don’t have a perfect solution. Tacrolimus is too effective to abandon. But its neurotoxicity is too common to ignore. New research is pointing toward smarter dosing. The TACTIC trial, launching in 2024, is testing a new algorithm that combines CYP3A5 genetics, magnesium levels, and blood pressure control to predict and prevent neurotoxicity before it starts. There’s also a new drug in the pipeline-LTV-1. Designed to have less access to the brain, it’s entering phase 2 trials in 2023. If it works, it could replace tacrolimus for many patients by 2027. Until then, the best defense is awareness. Know your symptoms. Track your levels. Ask about your genetics. Don’t let a tremor or headache be brushed off as "normal." Your brain matters just as much as your new organ.Real Stories, Real Impact
One kidney transplant patient, "KidneyWarrior42," reduced their tacrolimus dose from 0.1 mg/kg to 0.07 mg/kg and saw their tremor vanish in 72 hours. Another, "LiverSurvivor," spent months with daily headaches until they switched to cyclosporine. "It was like a fog lifted," they wrote. These aren’t rare cases. They’re the norm. And they’re preventable-if we listen.Can you have tacrolimus neurotoxicity even if your blood level is normal?
Yes. Neurotoxicity can occur even when tacrolimus blood levels are within the therapeutic range. About 30% of patients who develop symptoms have levels that are considered safe by standard guidelines. This is because individual differences in the blood-brain barrier and genetics (like CYP3A5 variants) affect how much drug reaches the brain-not just how much is in the bloodstream.
What’s the most common neurological symptom of tacrolimus toxicity?
Tremor is the most common symptom, affecting 65-75% of patients who experience neurotoxicity. It often starts as a fine shaking in the hands and can progress to interfere with daily tasks like eating, writing, or holding objects. Headache is the second most common, followed by insomnia and tingling sensations.
Which transplant patients are most likely to get tacrolimus neurotoxicity?
Liver transplant recipients have the highest risk, with about 35.7% developing neurotoxic symptoms. This is likely because the liver metabolizes tacrolimus, and a new liver may process the drug differently than the old one, causing unpredictable blood levels. Kidney transplant patients follow at 22.4%, then lung (18.9%) and heart (15.2%).
Can low sodium cause neurotoxicity with tacrolimus?
Yes. Hyponatremia (low sodium levels below 135 mmol/L) is a known risk factor. Studies show correcting sodium levels can resolve mild neurotoxicity in up to 28% of cases without needing to change the tacrolimus dose. This is why electrolyte checks are just as important as drug level monitoring.
Is there a genetic test that can help prevent tacrolimus neurotoxicity?
Yes. Testing for the CYP3A5 gene can identify whether you’re a fast or slow metabolizer of tacrolimus. Fast metabolizers break down the drug quickly and often need higher doses, which increases the risk of neurotoxicity. A 2021 study showed that using CYP3A5-guided dosing reduced neurotoxicity by 27%. While not yet standard everywhere, this testing is becoming more available at major transplant centers.
What should I do if I develop tremor or headache after a transplant?
Don’t wait. Contact your transplant team immediately. Ask for a tacrolimus blood level check, a sodium level test, and a review of all other medications you’re taking. Avoid stopping tacrolimus on your own-this can trigger rejection. Most symptoms improve with a small dose reduction (10-20%) or switching to cyclosporine, and improvement often happens within a few days.
Can other drugs make tacrolimus neurotoxicity worse?
Yes. Several common medications can increase the risk, especially those that affect the nervous system. These include antibiotics like linezolid, sedatives like midazolam or propofol, and antipsychotics like risperidone or olanzapine. Always tell your doctors you’re on tacrolimus before starting any new medication-even over-the-counter ones.


Stephen Tulloch
January 16, 2026 AT 15:14Bro, I’ve been on tacrolimus since my liver transplant in ’21 and yeah, the tremor was wild. Felt like my hands were doing the cha-cha without my permission 😅
But here’s the kicker - my doc kept saying ‘it’s fine, your levels are perfect’ until I demanded a CYP3A5 test. Turns out I’m a fast metabolizer. Dose dropped 15%, tremor gone in 4 days. Why are we still flying blind with just blood levels? 🤦♂️
Joie Cregin
January 17, 2026 AT 14:38My sister went through this after her kidney transplant - tremors so bad she couldn’t hold her coffee. We thought it was anxiety… until she screamed at the mirror one night, ‘Why is my hand moving like it’s possessed?!’ 😭
They finally checked her sodium and it was 129. Fixed that, kept the dose, and boom - she’s back to baking pies. Your brain deserves love too, not just your new organ 💛
Melodie Lesesne
January 19, 2026 AT 09:55I just want to say thank you for writing this. I’ve been silent about my tremor for months because I didn’t want to sound ‘weak’ or ‘ungrateful’ for having a new kidney.
But reading this? It’s like someone finally said it out loud. I’m scheduling an appointment tomorrow to ask about my CYP3A5 status. No more guessing. 💪
Corey Sawchuk
January 20, 2026 AT 05:48Had the headache for 3 weeks. Took everything. Nothing worked. Then I remembered I’d started taking melatonin for sleep. Looked it up - yep, interacts with tacrolimus.
Stopped it. Headache lifted in 48 hours. Simple fix. Why don’t they tell you this stuff upfront?
Also, low sodium = real. My doc didn’t even check it until I asked. 🤷♂️
Cheryl Griffith
January 21, 2026 AT 16:11This is so important. I’m a nurse who works with transplant patients and I’ve seen too many dismissed as ‘just stressed’ or ‘having bad sleep.’
Neurotoxicity isn’t a personality flaw - it’s a pharmacological reality. We need better education for both patients and providers. Thank you for putting this out there.
Kasey Summerer
January 22, 2026 AT 19:27So let me get this straight - we’ve got this miracle drug that keeps you alive… but also turns your brain into a glitchy PlayStation 2?
And we still don’t test your genes before dosing it? 😂
Next thing you know, they’ll prescribe a Tesla to fix your liver and wonder why you’re crying in the garage.
Also, CYP3A5? Sounds like a secret society. Who’s in charge here - a wizard?
kanchan tiwari
January 24, 2026 AT 18:13THEY KNOW. THEY’VE ALWAYS KNOWN. That’s why they call it ‘Tacrolimus’ - TACRO-LIMUS… TACRO = TACO, LIMUS = LIMB? No. LIMUS = LIMBO.
They’re keeping you in limbo so you’ll keep taking the pills. The FDA, Big Pharma, transplant centers - they’re all in on it.
They don’t want you to know about CYP3A5 because if you do, you’ll demand personalized dosing and they’ll lose billions.
And don’t get me started on PRES - they call it ‘reversible’ like that’s comforting when half the people who get it end up in a coma. 🚨
Bobbi-Marie Nova
January 25, 2026 AT 14:28Okay but imagine if your car’s engine light came on and the mechanic said ‘nah, your gas tank is full, you’re fine’ - even though the car’s shaking and smoking?
That’s what this is. We treat tacrolimus like it’s a magic bullet and ignore the dashboard.
Also, I switched to cyclosporine and my headaches vanished. Not perfect, but I can finally sleep through the night. And yes, I cried. Happy tears this time. 🥹
Allen Davidson
January 27, 2026 AT 13:40Just wanted to add - if you’re reading this and you’re scared or overwhelmed, you’re not alone. I’ve been there. Tremor, insomnia, the whole package.
But you’re not weak for needing help. You’re not ungrateful for wanting to feel normal again.
Advocate for yourself. Ask for the sodium test. Ask for the gene test. Push for a dose tweak. Your brain is worth fighting for - and you’ve already survived the transplant. This is just the next step.
You got this. 💪