MH Dantrolene Dosage Calculator
This calculator determines the correct initial dose of dantrolene for malignant hyperthermia (MH) treatment based on patient weight. The initial dose is 2.5 mg per kilogram of body weight, with a maximum of 10 mg/kg.
Recommended Dose
Equivalent to vials (each containing 20 mg)
When you walk into a hospital for surgery, you trust that the team will keep you safe. But there’s a rare, hidden danger lurking in some anesthetic drugs - one that can turn a routine procedure into a medical emergency within minutes. This is malignant hyperthermia (MH), a severe, life-threatening reaction that strikes without warning in genetically susceptible people. It doesn’t care if you’re young, fit, or have never had a problem with anesthesia before. One moment you’re stable; the next, your body is overheating, your muscles are locking up, and your organs are under siege.
What Triggers Malignant Hyperthermia?
Malignant hyperthermia isn’t caused by infection, trauma, or poor care. It’s triggered by specific drugs used in general anesthesia. The two biggest culprits are volatile anesthetic gases - sevoflurane, desflurane, and isoflurane - and the muscle relaxant succinylcholine. These are common in surgeries from tonsillectomies to hip replacements. If you carry a mutation in the RYR1 gene (found in about 70% of cases), your muscle cells react abnormally when exposed to these drugs. Instead of releasing calcium in controlled bursts, your cells flood with it, causing muscles to contract nonstop. That constant contraction burns through oxygen and generates massive amounts of heat - your body temperature can spike to 109°F (43°C) in under an hour.
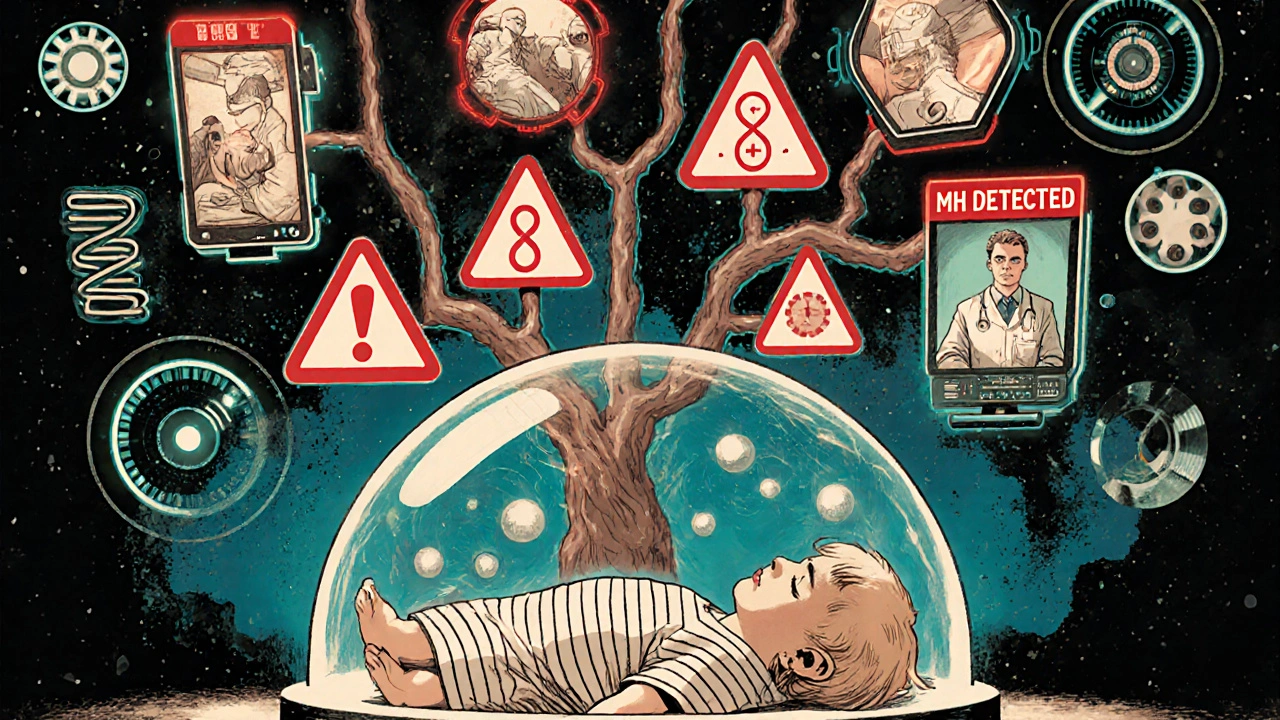
It’s not just about the drugs. The risk is inherited. If a parent or sibling has had MH, your chance of carrying the mutation is much higher. But here’s the catch: 29% of MH cases happen in people with no known family history. That means even if your relatives never had a problem, you could still be at risk. This is why experts now say you can’t rely on family history alone to rule out danger.
How Do You Know It’s Happening?
The signs don’t wait for a patient to wake up. They show up during surgery, often within minutes of the anesthetic being given. The earliest warning is usually a sudden, unexplained rise in heart rate - over 120 beats per minute in adults. That’s followed by a spike in carbon dioxide (ETCO2) in the breath, often above 55 mmHg. This happens because your muscles are working nonstop, burning through oxygen and producing CO2 faster than your lungs can clear it.
Then comes muscle rigidity, especially in the jaw. Anesthesiologists call this masseter muscle rigidity - when the patient’s jaw locks tight after succinylcholine is given. It’s a classic red flag. Within minutes, body temperature begins to climb. By the time it hits 104°F, the situation is critical. Blood tests will show acidosis (pH below 7.2), high potassium (over 5.5 mEq/L), and skyrocketing creatine kinase - often over 10,000 U/L - as muscle tissue breaks down. The urine turns dark brown or red from myoglobin, a sign your kidneys are under threat.
These symptoms can appear as early as 3 minutes after the trigger or as late as 24 hours after surgery, though most happen within the first hour. The longer it goes untreated, the worse it gets. Without quick action, multi-organ failure and death follow.
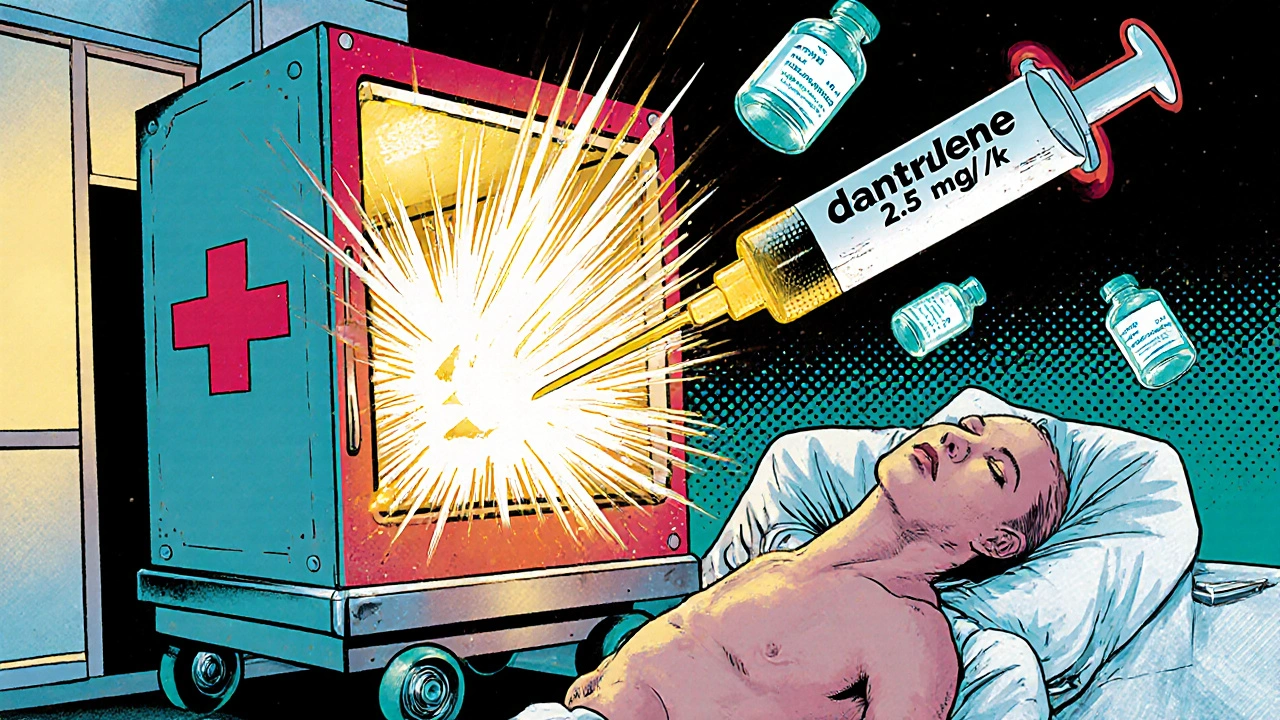
The Only Treatment That Works: Dantrolene
There is no guesswork in treating MH. The only drug that reverses the reaction is dantrolene. It works by blocking the abnormal calcium release in muscle cells, stopping the runaway contraction. But timing is everything. If dantrolene is given within 20 minutes of the first signs, survival rates jump to nearly 100%. Delay it past 40 minutes, and the chance of death climbs to 50%.
There are two forms: Dantrium® and Ryanodex®. Ryanodex®, approved in 2014, is now the standard. It comes as a powder that reconstitutes in just one minute - compared to 22 minutes for Dantrium®. That’s a game-changer in an emergency. Each vial contains 20 mg of dantrolene. The initial dose is 2.5 mg per kilogram of body weight - that’s about 175 mg for a 70 kg adult. But you don’t stop there. You keep giving more every 5 to 10 minutes until the symptoms stop. The maximum initial dose is 10 mg/kg, which means a single adult might need up to 700 mg - or 35 vials.
Hospitals are required to keep at least 36 vials on hand - enough for one adult case - at a cost of around $144,000. That’s expensive, but not as expensive as a death. In rural hospitals, stockouts still happen. In 2022, 22% of rural facilities reported running out of dantrolene. That’s not just a supply issue - it’s a safety failure.
What Else Happens During an MH Crisis?
Dantrolene is the star, but it’s not the whole team. Once MH is suspected, the anesthesiologist must immediately stop all triggering anesthetics. They switch to 100% oxygen at 10 liters per minute and hyperventilate the patient to flush out CO2. Surgery is canceled, even if it’s halfway done. The patient is cooled aggressively - ice packs on the neck, armpits, and groin; cold IV fluids; sometimes even cardiopulmonary bypass in extreme cases.
High potassium can cause fatal heart rhythms, so insulin and glucose are given to drive potassium back into cells. Acidosis is treated with sodium bicarbonate. To protect the kidneys from myoglobin damage, doctors give mannitol and furosemide. Blood gases, electrolytes, and CK levels are checked every 15 to 30 minutes. The patient often needs intensive care for days after the crisis.
Why Do Some Hospitals Fail?
It’s not about lack of knowledge. Most anesthesiologists know the protocol. The problem is preparedness. In 2022, a survey found only 63% of rural surgical centers followed the full MH emergency protocol. Academic hospitals? Nearly 100%. Why the gap? Cost, staffing, training.
Every operating room should have an MH cart - stocked with dantrolene, sterile water, syringes, needles, cooling gear, and blood gas kits. It must be checked quarterly. Staff need annual simulation drills. A 2021 study found residents need at least three mock MH scenarios before they can reliably spot the signs. Many facilities skip these drills. Some don’t even have a designated MH cart.
And then there’s the human factor. In one case shared on an anesthesiology forum, a doctor noticed a jaw spasm and rising ETCO2 but hesitated - thinking it was just a normal reaction. By the time he called for dantrolene, the patient’s temperature was 107°F. He survived, but barely. That’s the danger: if you don’t act fast, you’re betting your patient’s life on luck.
What About Genetic Testing?
If you’ve had MH or have a family history, genetic testing for RYR1 mutations is available. The test costs between $1,200 and $2,500 and has 95% sensitivity for known mutations. But it’s not perfect. Not every mutation is known yet. A negative test doesn’t guarantee safety. That’s why the gold standard for diagnosis remains the in vitro contracture test (IVCT), where a muscle biopsy is exposed to triggering agents in a lab. It’s invasive, expensive, and only done at specialized centers.
Still, testing is growing. Twenty-seven U.S. labs now offer RYR1 screening. The European Malignant Hyperthermia Group updated its IVCT criteria in January 2023 to detect even milder cases. If you’re planning surgery and have a family history, ask about testing. It could save your life.
The Future of MH Management
The biggest breakthroughs are coming fast. In 2024, the FDA is expected to approve an intranasal form of dantrolene - something that could be given in ambulances or ERs before the patient even reaches the OR. Clinical trials are underway for new drugs like S107, which stabilize the ryanodine receptor and may prevent MH before it starts. Long-term, CRISPR gene editing could one day correct the RYR1 mutation itself - Phase I trials are projected for 2027.
Already, anesthesia machines are getting smarter. Epic Systems’ 2024 update includes AI-driven alerts that trigger when three MH indicators appear together: rising CO2, fast heart rate, and high temperature. That’s not science fiction - it’s happening now. These systems can flag danger before a human even notices.
What Should You Do?
If you’re scheduled for surgery:
- Ask if your hospital has a full MH emergency kit and if staff are trained in MH protocols.
- If you or a close relative has had a bad reaction to anesthesia, ask about genetic testing.
- Don’t assume you’re safe just because you’ve had anesthesia before - MH can strike the first time.
- Keep a written record of any anesthesia reactions - even if they seemed minor.
If you’re a patient or family member, know this: malignant hyperthermia is rare, but it’s real. And it’s treatable - if caught early. The difference between life and death often comes down to a single question: Is dantrolene ready? Is the team ready? If the answer isn’t a confident yes, it’s worth asking.
Can malignant hyperthermia happen during local anesthesia?
No, malignant hyperthermia only occurs with general anesthesia involving triggering agents like sevoflurane, desflurane, isoflurane, or succinylcholine. Local anesthetics like lidocaine or nerve blocks do not cause MH. However, if you’re having a procedure under general anesthesia - even briefly - you’re at risk if you carry the genetic mutation.
Is malignant hyperthermia the same as heat stroke?
No. While both involve dangerously high body temperature, heat stroke is caused by environmental overheating or physical exertion. Malignant hyperthermia is a genetic, drug-induced reaction that starts internally due to uncontrolled muscle contractions. The treatment is completely different - dantrolene works for MH but not for heat stroke.
Can you outgrow malignant hyperthermia?
No. Malignant hyperthermia is caused by a lifelong genetic mutation. Once you have the RYR1 or CACNA1S gene variant, you’ll always be at risk when exposed to triggering anesthetics. There’s no cure, no remission - only avoidance and preparedness.
What if I don’t know my family history?
That’s more common than you think. Nearly one-third of MH cases occur in people with no known family history. If you’re having surgery and have no way to confirm your genetic risk, the best approach is to ask your anesthesiologist to avoid triggering agents. Non-triggering anesthetics like propofol, ketamine, and regional blocks are safe alternatives.
Are children more at risk for malignant hyperthermia?
Yes. Children, especially those under 15, have a higher incidence - about 1 in 3,000 anesthetics compared to 1 in 50,000 in adults. Tonsillectomies and adenoidectomies are common triggers because they often use succinylcholine. Pediatric hospitals are now required to have MH protocols in place, and many avoid succinylcholine entirely in kids unless absolutely necessary.
Can I get tested for malignant hyperthermia before surgery?
Yes, but it’s not routine. Genetic testing for RYR1 mutations is available and costs between $1,200 and $2,500. The in vitro contracture test (IVCT) is more accurate but requires a muscle biopsy and is only done at specialized centers. Testing is recommended if you or a close relative had a previous MH reaction or unexplained death during anesthesia. If you’re unsure, talk to your doctor or an anesthesiologist before your procedure.
Final Thought: Preparedness Saves Lives
Malignant hyperthermia is rare, but it doesn’t need to be deadly. The tools to save lives exist - dantrolene, training, protocols, and awareness. The problem isn’t science. It’s systems. A single hospital’s failure to stock dantrolene, skip training, or ignore early signs can turn a preventable reaction into a tragedy. If you’re facing surgery, don’t assume safety. Ask the questions. Demand readiness. Because when it comes to MH, the difference between life and death isn’t luck - it’s preparation.

Deepak Mishra
November 15, 2025 AT 03:22OMG this is wild!!! I knew someone who had a jaw lock after surgery and they said it was just stress but now I think it was MH???!!! My cousin died after a tonsillectomy in 2010 and they said it was 'complications' but what if it was this??? I’m never going under again unless they test me first!!! 😱
Rachel Wusowicz
November 16, 2025 AT 02:00They’re hiding the truth… the pharmaceutical companies know about MH, they’ve known for decades, but they won’t make dantrolene cheaper because they profit off the panic. And why is Ryanodex so expensive? Because they’ve got a monopoly. The FDA? Complicit. The real danger isn’t the gene-it’s the system that lets hospitals run out of life-saving drugs because of ‘budget constraints.’
They don’t want you to know that 90% of MH deaths happen in places that didn’t even have the cart stocked. It’s not medical-it’s corporate negligence dressed up as ‘rare.’
And don’t get me started on the AI alerts… they’re just there to make you feel safe while the real solution-mandatory testing and non-triggering protocols-is ignored. Wake up. This isn’t science. It’s a profit-driven cover-up.
John Mwalwala
November 17, 2025 AT 01:42Let me break this down for you in proper clinical terms: RYR1 mutations cause calcium dysregulation via sarcoplasmic reticulum dysfunction, which triggers uncontrolled ryanodine receptor 1 channel activation leading to sustained muscle contraction, hypermetabolism, and thermogenesis. It's not 'overheating'-it's a cellular cascade failure. And yes, succinylcholine is the classic trigger because it depolarizes the motor endplate, amplifying the calcium leak. You can't just say 'it's rare'-you need to understand the pathophysiology to prevent it.
Also, the 2.5 mg/kg dosing? That's outdated. The 2023 MHAUS guidelines recommend 2.5–10 mg/kg titrated to clinical response, and the median dose is actually 12 mg/kg in severe cases. Don't listen to the blog posts-read the peer-reviewed literature.
Latrisha M.
November 17, 2025 AT 14:31If you're scheduled for surgery, ask your anesthesiologist if they have dantrolene on hand and if they do MH drills. It's a simple question. If they hesitate or say 'it's rare,' that's a red flag. You don't need to be paranoid-just informed. And if you have a family history, get tested. It's not expensive compared to what could happen.
Also, local anesthesia is perfectly safe. No need to fear every procedure. Just know your risks and ask the right questions. You're your own best advocate.
Jamie Watts
November 19, 2025 AT 11:38People are so dramatic about this. I've had five surgeries and never had an issue. You think your jaw spasm was MH? Nah. Probably just nervous tension. And why are you paying $2500 for a genetic test when you can just avoid succinylcholine and volatile gases? Duh. Any decent anesthesiologist knows not to use those in high-risk cases. Stop panicking. Just tell your doctor you want propofol and regional. Done. No drama.
Also, dantrolene isn't that hard to get. If your hospital doesn't have it, go somewhere that does. You think hospitals are gonna let you die? Please. They're not that incompetent.
David Rooksby
November 20, 2025 AT 09:28Let me tell you something you won't hear from the medical establishment-this whole MH thing is just the tip of the iceberg. The real issue is that anesthesia has been weaponized. They use these triggering agents because they're cheap, they're fast, and they make the procedure look easy for the residents. But they don't care about the long-term genetic fallout. You think they're worried about your kids inheriting RYR1? No. They're worried about liability and insurance premiums. So they tell you it's 'rare' and move on. But here's the truth: every time you're put under, you're rolling the dice with your DNA. And the system doesn't want you to know that. That's why they don't screen everyone. That's why they don't fund CRISPR trials faster. That's why they let rural hospitals run out of dantrolene. Because if everyone knew how fragile this is, they'd demand change. And change costs money. And money? That's what they're protecting.
Daniel Stewart
November 21, 2025 AT 17:58Isn't it ironic? We live in an age where we can edit genes, predict cancer from a drop of blood, and send robots to Mars… but we still let people die from a reaction we’ve known about since the 1960s? We have the tools. We have the knowledge. But we lack the moral courage to act. MH isn't a medical anomaly-it's a mirror. It reflects our collective indifference to systemic failure. We'd rather blame genetics than fix the system. We'd rather call it 'rare' than fund the carts. We'd rather wait for someone to die before we do something. And that… that is the true tragedy.
Diane Tomaszewski
November 23, 2025 AT 01:53I had a cousin who had MH during a wisdom tooth removal. She survived because the anesthesiologist recognized the jaw tightness right away. They gave dantrolene and cooled her down. She's fine now. But I never knew until after. So if you're having surgery, just ask. It's not scary. It's smart. And if they say no, find a different hospital. That's all.