Most people think of a medication overdose as a one-time emergency - a scary moment in the ER, maybe a dose of naloxone, and then home again. But for many survivors, the real story doesn’t end when they leave the hospital. The damage doesn’t always show up right away. Sometimes, it creeps in months later - in the way you can’t remember your child’s name, how you stumble walking down the stairs, or how even simple decisions feel impossible. This isn’t rare. It’s the new normal for too many who survive.
Brain Damage Isn’t Always Obvious - But It’s Common
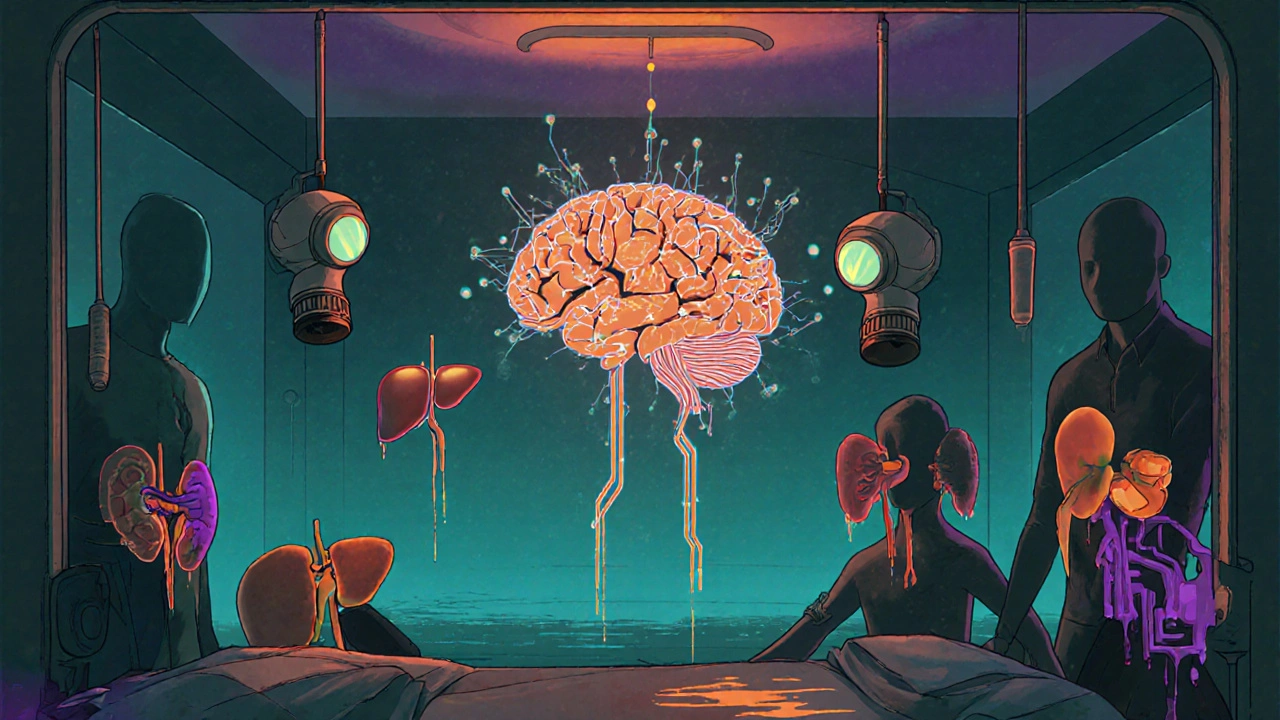
When you overdose on opioids, benzodiazepines, or even too much acetaminophen, your body shuts down. Breathing slows. Oxygen stops reaching your brain. And it doesn’t take long for that to cause permanent harm. After just four minutes without enough oxygen, brain cells start dying. The longer it goes on, the worse it gets. A 2023 clinical analysis found that 63% of overdose survivors struggle with memory loss - both short-term and long-term. Another 57% report trouble concentrating. These aren’t vague complaints. They’re measurable, persistent changes in brain function. One survivor on Reddit wrote: "Two years later, I still can’t remember conversations from 10 minutes ago." That’s not just forgetfulness. That’s brain injury. The damage isn’t always the same. Some people lose motor control - 38% report trouble with balance or coordination. Others can’t speak clearly. Twenty-nine percent have lasting speech problems. And it’s not just physical. The part of your brain that makes decisions, plans ahead, or solves problems? That gets hit too. Over 30% of survivors say they can’t think clearly enough to make even small choices. What’s worse? This isn’t just from opioids. Benzodiazepine overdoses - like taking too many Xanax or Valium - lead to cognitive fog that lasts over six months in nearly a third of cases. Stimulant overdoses, like from Adderall or Ritalin, can permanently alter brain chemistry, leading to chronic anxiety or even psychosis. And acetaminophen? It doesn’t affect the brain directly, but it kills the liver. Forty-five percent of people who wait more than eight hours to get treatment end up with cirrhosis or other lasting liver damage.Your Organs Don’t Just Bounce Back
The brain isn’t the only system that pays the price. Every overdose is a shock to your entire body. Opioid overdoses cause respiratory depression - your lungs stop working well enough to oxygenate your blood. That lack of oxygen doesn’t just hurt your brain. It damages your kidneys, heart, and nerves too. Studies show that 22% of overdose survivors develop kidney failure. Eighteen percent have heart complications - irregular rhythms, high blood pressure, even heart attacks. Fifteen percent get fluid in their lungs. Eight percent suffer strokes. And if you vomit while unconscious, you can inhale it - leading to pneumonia, which then becomes a chronic issue. The damage is often silent at first. You feel fine. You’re discharged. But months later, you’re tired all the time, your kidneys aren’t filtering right, or you’re short of breath climbing stairs. These aren’t "side effects" - they’re direct results of the overdose. And they don’t go away on their own.The Mental Health Toll Is Just as Real
Surviving an overdose doesn’t just leave physical scars. It leaves emotional ones. Over 70% of survivors develop a new mental health condition afterward. Forty-one percent get PTSD from the experience of nearly dying. Thirty-eight percent develop major depression. Thirty-three percent battle chronic anxiety. This isn’t just sadness. It’s a deep, persistent trauma. One person described it as "walking through fog every day." They’re not being dramatic. Their brain chemistry changed. Their sense of safety was shattered. And without proper support, that trauma becomes part of their daily life. Worse, only 28% of survivors get mental health care within 30 days of their overdose. That’s not a coincidence. The system treats the overdose like an accident - not the start of a long-term health crisis. But your mind doesn’t recover just because your breathing did.
Why So Many People Are Left Behind
Here’s the hard truth: most hospitals don’t know what to do after the overdose is reversed. A 2022 review found that only 47% of emergency rooms document any plan for long-term monitoring. And 41% of survivors are sent home without a single referral for follow-up care. Even when they’re told to come back, they don’t. Why? Because the system doesn’t make it easy. There are no clear pathways. No specialists waiting. No coordinated care. In 69% of U.S. counties, there’s no access to neurological rehab for overdose survivors. That means if you’re left with memory loss, balance problems, or trouble thinking - you’re on your own. And then there’s the timing problem. With acetaminophen, you have just eight hours to get treatment before liver damage becomes permanent. But 32% of people don’t arrive at the hospital until it’s too late - because they don’t feel sick yet. The symptoms don’t show up for two to three days. So they wait. And by then, it’s too late.What’s Being Done - And What’s Not
There’s some progress. In 2023, the Biden administration allocated $156 million to study hypoxic brain injury from overdoses - the first federal funding focused on long-term outcomes. The American Medical Association now requires doctors to do neurological assessments within 72 hours of an overdose. That’s a step forward. But the gaps are still massive. Only 19% of U.S. hospitals have formal protocols for managing long-term effects. The National Safety Council says current funding for this research is 87% below what experts say is needed. And by 2030, unless things change, only 22% of survivors will get the care they need. The cost? The average lifetime healthcare cost for someone with permanent brain damage from an overdose is over $1.2 million. That’s not just money. It’s lost jobs, broken relationships, and a lifetime of disability.

Edward Hyde
November 29, 2025 AT 22:30So let me get this straight - we’re now treating overdoses like chronic illnesses? Cool. Meanwhile, my cousin OD’d on oxycodone last year and got kicked out of rehab for ‘not being motivated enough.’ The system’s a circus, and we’re all paying for front-row seats to the clown show. Brain damage? Sure. But who’s gonna pay for the MRI when your insurance says ‘pre-existing condition’? I’ve seen this movie before. It ends with a bill and a shrug.
Charlotte Collins
December 1, 2025 AT 00:42The data here is chilling, but not surprising. What’s more disturbing is how little the medical establishment has adapted. We treat overdoses as emergencies because that’s the only frame we have - acute, reactive, disposable. But the body doesn’t reset. The brain doesn’t reboot. The liver doesn’t auto-repair. And yet, we discharge people with a pamphlet and a prayer. This isn’t negligence. It’s institutionalized abandonment disguised as efficiency.
Margaret Stearns
December 1, 2025 AT 08:09i just read this and cried. my brother survived an acetaminophen overdose and now he gets tired after walking to the mailbox. no one told us the liver damage would last forever. thank you for saying this out loud.
amit kuamr
December 2, 2025 AT 16:30Scotia Corley
December 3, 2025 AT 09:07While the emotional weight of this post is undeniable, it lacks rigorous statistical contextualization. The 63% memory loss figure, for instance, fails to specify whether it refers to clinically diagnosed amnestic syndromes or self-reported cognitive complaints. Furthermore, the conflation of correlation with causation in organ damage attribution undermines the credibility of the argument. Until peer-reviewed longitudinal studies confirm these claims, we risk pathologizing a subset of acute medical events as chronic conditions.
elizabeth muzichuk
December 3, 2025 AT 18:53Let me be clear: if you overdose, you made a choice. You chose to ignore warnings. You chose to numb yourself. Now you want the whole world to pay for your consequences? You think brain damage is tragic? Try being the child who watches their parent forget their name. Try being the spouse who has to relearn how to love someone who’s still here but gone. This isn’t a medical crisis - it’s a moral one. And nobody wants to talk about the sin behind the symptom.
Debbie Naquin
December 3, 2025 AT 19:08What we’re observing here isn’t merely iatrogenic harm - it’s a systemic epistemic failure. The biomedical model operates on a binary: alive/dead, functional/dysfunctional. But hypoxic injury introduces a third state: the persistently altered. A neurophenomenological shift that defies diagnostic taxonomy. We lack the linguistic and institutional scaffolding to map the lived experience of post-overdose cognition. The $156M funding is a start, but without phenomenological research - without listening to survivors as epistemic agents - we’re just mapping symptoms without understanding the substrate of suffering.