For people with severe asthma who still struggle to breathe despite using inhalers, steroids, and other standard treatments, there’s a different kind of medicine that’s changing lives: biologics. These aren’t your typical pills or inhalers. They’re lab-made antibodies designed to block specific parts of the immune system that go haywire in asthma. Two of the most important classes are anti-IgE and anti-IL-5 therapies. If you’ve been told your asthma is "difficult to control," these drugs might be worth talking about.
What Makes Biologics Different?
Most asthma treatments work broadly - they reduce inflammation or open airways. Biologics are precise. They target one molecule at a time, like a sniper instead of a shotgun. Omalizumab (Xolair) blocks IgE, the antibody that triggers allergic reactions. Mepolizumab (Nucala), reslizumab (Cinqair), and benralizumab (Fasenra) all block IL-5, a protein that tells eosinophils - a type of white blood cell - to swarm the lungs and cause swelling. These drugs don’t fix asthma overnight. But for the right person, they can slash flare-ups by half or more.Anti-IgE: Omalizumab and Allergic Asthma
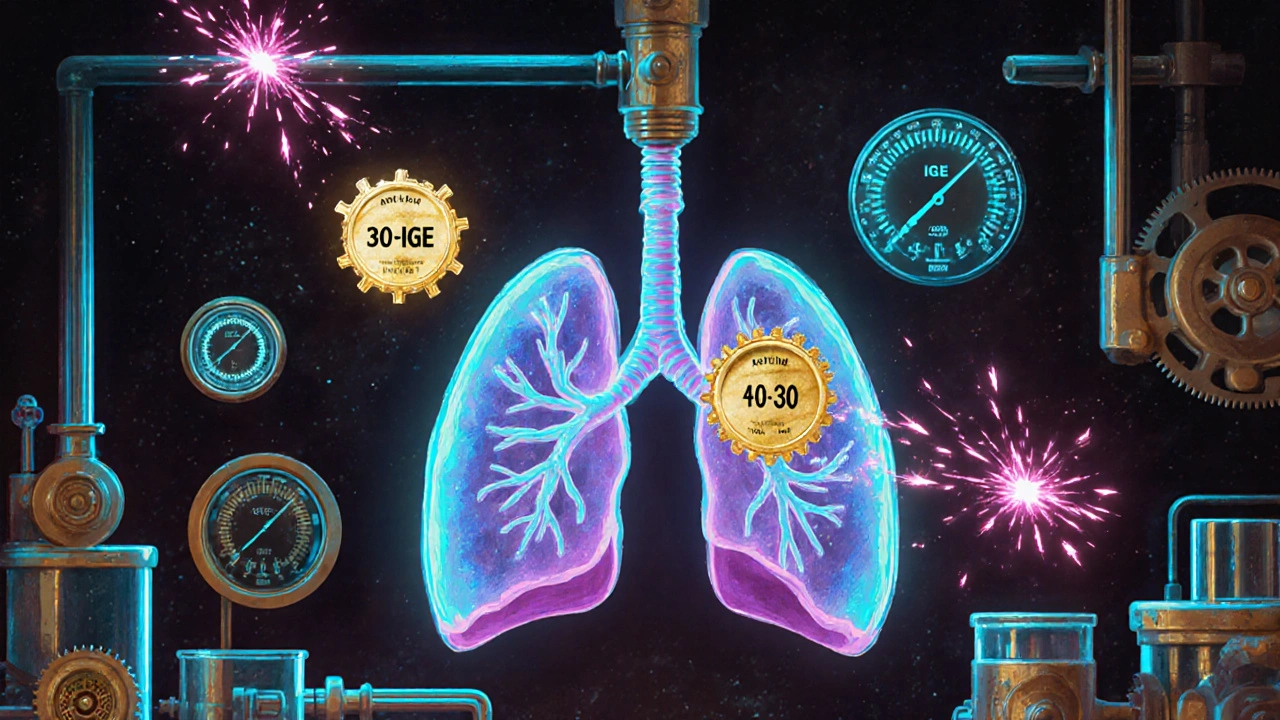
Omalizumab was the first biologic approved for asthma back in 2003. It’s still widely used today. This drug works best if your asthma is tied to allergies. That means you react to dust mites, pet dander, or pollen. Your doctor will check your blood for IgE levels and do skin tests to confirm you’re allergic to something. If your IgE is between 30 and 1500 IU/mL and you’re over 6 years old, you might be a candidate. The goal? Stop IgE from attaching to mast cells and basophils - the cells that release histamine and cause wheezing, coughing, and tightness. When IgE can’t bind, the allergic chain reaction doesn’t start. Studies show omalizumab cuts asthma attacks by about 50% in people who fit this profile. It’s given as a shot under the skin every 2 to 4 weeks. Some people get mild redness or itching at the injection site. Rarely, there’s a risk of anaphylaxis - about 1 in 1,000 doses - so you’re usually monitored for 30 minutes after the first few shots. One thing to know: omalizumab doesn’t work during an active asthma flare. It’s for prevention. You still need your rescue inhaler.Anti-IL-5: Targeting Eosinophilic Asthma
If your asthma isn’t driven by allergies, it might be driven by too many eosinophils. These cells build up in the airways, causing chronic inflammation that doesn’t respond well to steroids. That’s where anti-IL-5 drugs come in. Mepolizumab and reslizumab bind directly to IL-5, the signal that tells eosinophils to multiply. Benralizumab goes one step further - it attaches to the IL-5 receptor on eosinophils and literally kills them. Within 24 hours, blood eosinophil counts can drop by over 95%. That’s faster and deeper than the others. To qualify, your blood test needs to show at least 150 eosinophils per microliter, or 300 in the past year. These drugs are for people with persistent symptoms, frequent hospital visits, or steroid dependence. In clinical trials, mepolizumab reduced flare-ups by 52%. Benralizumab did the same - 51%. Reslizumab is given as an IV infusion every 4 weeks, while the others are injections. Side effects are usually mild: headache, sore throat, or injection site reactions. But some people report joint pain or fatigue. One patient on Reddit said benralizumab caused severe joint pain after three doses - enough to stop it. That’s rare, but it happens.
Who Benefits the Most?
Not everyone with severe asthma responds to biologics. About 30-40% of patients don’t see much improvement. That’s why matching the drug to the biology matters. - If you have allergies + high IgE → omalizumab is your best bet. - If you have high eosinophils + no clear allergies → mepolizumab, reslizumab, or benralizumab are better choices. - If you’ve tried other biologics and still flare up → tezepelumab (which blocks TSLP, an upstream trigger) might help, even if your eosinophils are low. Doctors don’t guess anymore. They test. Blood eosinophils, IgE levels, FeNO (fractional exhaled nitric oxide), and asthma control scores are all part of the decision. You also need to prove you’re using your inhalers correctly and consistently. Many people think they’re taking their meds right - but studies show up to half aren’t.What to Expect After Starting
These aren’t quick fixes. Some people feel better in 4 to 6 weeks. Others take 3 to 4 months. You won’t wake up one day breathing perfectly. But over time, you might notice fewer nights woken by coughing, less reliance on oral steroids, and fewer ER visits. Real-world data shows 65% of patients can reduce or stop taking daily prednisone. That’s huge. Long-term steroid use causes weight gain, bone loss, diabetes, and mood swings. Cutting that out improves quality of life more than most people realize. A 2023 survey by the American College of Allergy found 78% of biologic users felt their quality of life improved. One patient on r/asthma wrote: “After 6 months on mepolizumab, I went from 3-4 ER visits a year to zero. I haven’t needed prednisone in 14 months.”
Cost and Access
These drugs are expensive. Annual costs range from $25,000 to $40,000 USD. Insurance rarely covers them without prior authorization - and that process can take 2 to 3 weeks. Some manufacturers offer co-pay assistance programs that bring out-of-pocket costs down to under $50 per month for eligible patients. Access varies. In the U.S., about 2% of eligible patients get biologics. In Europe, it’s 1.4%. In Asia, less than 1%. Part of the problem is cost. Part is awareness. Many primary care doctors still don’t know when to refer.Challenges and Limitations
Biologics aren’t perfect. You need regular shots or infusions. You need ongoing blood tests. You need to stay on your inhalers. And if your asthma changes - say, you get a lung infection or stop being allergic - the drug might stop working. Also, we don’t know what happens after 10 years of use. Long-term safety data is still being collected. The European Respiratory Society says we need better ways to predict who will respond - not just by eosinophils or IgE, but by genetics, lung tissue markers, or even gut microbiome changes.What’s Next?
The field is moving fast. New biologics like tezepelumab (Tezspire) work earlier in the inflammation chain, helping people even if their eosinophils are normal. Trials are testing biologics that only need to be injected twice a year. There’s even research into oral versions - though none are approved yet. The goal isn’t just to reduce attacks. It’s to let people live without fear. To play with their kids. To sleep through the night. To not carry an EpiPen just in case. For the right person, these drugs aren’t just treatment - they’re freedom.How do I know if I’m a candidate for anti-IgE or anti-IL-5 biologics?
Your doctor will check your asthma history, how often you’ve had flare-ups or hospital visits, and whether you still rely on oral steroids. Blood tests for eosinophils and IgE levels are required. Skin or blood allergy tests help determine if your asthma is allergic. If your eosinophil count is above 150 cells/μL, anti-IL-5 drugs may help. If you have allergies and IgE between 30-1500 IU/mL, omalizumab could be right for you. You must also prove you’re using your inhalers correctly and consistently.
How long does it take for biologics to start working?
Some people notice less coughing or fewer nighttime symptoms within 4 to 6 weeks. But full benefits - like fewer hospital visits or less steroid use - often take 3 to 6 months. Don’t stop if you don’t feel better right away. These drugs build up slowly in your system.
Can I stop my inhalers if I start a biologic?
No. Biologics are add-on therapies. You still need your daily controller inhaler (usually an inhaled corticosteroid) and your rescue inhaler (like albuterol). They work together. Stopping your regular meds can lead to dangerous flare-ups.
Are there serious side effects?
Most side effects are mild: sore throat, headache, or redness at the injection site. These usually fade after a few doses. A rare but serious risk is anaphylaxis - about 1 in 1,000 doses. You’ll be monitored after your first few shots. If you’ve had severe allergic reactions before, your risk is higher. Joint pain and fatigue have been reported with benralizumab in some cases.
Why do some people stop biologics even when they help?
Cost and access are big reasons. Insurance delays can make starting treatment frustrating. Some people find the injection schedule hard to keep up with. Others experience side effects like joint pain or fatigue. A few realize they still need oral steroids and feel the trade-off isn’t worth it. It’s not failure - it’s finding what fits your life.
Is there a chance I won’t respond at all?
Yes. About 30-40% of people don’t get a meaningful benefit, even if they meet all the criteria. That’s why doctors use biomarkers - to improve the odds. But we’re still learning who responds best. If one biologic doesn’t work, switching to another class (like from anti-IgE to anti-IL-5) might help. Some patients respond better to tezepelumab if others failed.

Kathryn Ware
November 18, 2025 AT 00:36I started on omalizumab last year and wow 🤯 I went from 4 ER visits a year to zero. My nights are actually peaceful now. I used to wake up gasping like a fish on land, but now I sleep like a baby 😴 Even my dog notices the difference - she doesn’t have to nudge me awake anymore because I’m coughing. The shots are annoying, yeah, but they’re way better than prednisone bloat. My doctor said I’m a "perfect candidate" - allergies + high IgE. If you’re on the fence, just talk to an allergist. No regrets here 🌿💕
kora ortiz
November 18, 2025 AT 09:20Biologics aren’t magic they’re science and if you’re not getting them you’re leaving your life on the table
Jeremy Hernandez
November 19, 2025 AT 02:39LMAO so now we’re giving people expensive antibodies because Big Pharma wants to make more money? I’ve seen this movie before - remember the Vioxx scandal? They’ll tell you it’s revolutionary until the side effects show up in 5 years. My cousin was on benralizumab and ended up with joint pain so bad he couldn’t hold his grandkid. They don’t tell you that part on the TV ads. And don’t even get me started on the $40k price tag. This isn’t medicine it’s a luxury subscription.
Tarryne Rolle
November 20, 2025 AT 05:06Isn’t it strange how we’ve outsourced our immune systems to lab-made proteins? We used to endure - now we engineer. We used to adapt - now we delete. We call this progress but what are we becoming? If your body can’t handle asthma without a biologic, maybe the problem isn’t your lungs - maybe it’s your environment, your diet, your soul. We’ve turned medicine into a transaction with biology. And I wonder… who’s really paying the price?
Kyle Swatt
November 20, 2025 AT 17:15I used to think asthma was just wheezing and panic until I saw my sister on mepolizumab. She went from being a ghost in her own house to hiking mountains with her kids. These drugs don’t just treat symptoms - they give back time. Time to laugh. Time to breathe without fear. Time to be present. And yeah the shots suck and the cost is insane but when you’ve spent years counting breaths like they’re money… you’ll do anything to get your life back. This isn’t just science - it’s dignity.
Deb McLachlin
November 21, 2025 AT 03:41Thank you for this comprehensive overview. I appreciate the emphasis on biomarker-driven prescribing. However, I would urge clinicians to consider longitudinal tracking of FeNO levels alongside eosinophil counts, as recent studies suggest dynamic changes in fractional exhaled nitric oxide may predict non-response prior to clinical deterioration. Additionally, adherence to controller inhalers remains a critical confounder in real-world outcomes - perhaps a digital inhaler sensor program should be integrated into biologic eligibility protocols.
saurabh lamba
November 21, 2025 AT 13:17Why do rich countries spend so much on these drugs when people here can’t even get basic inhalers? 😔 We have asthma too. But no one cares. Biologics? Maybe in 20 years. For now, we pray.
Kiran Mandavkar
November 22, 2025 AT 17:45Pathetic. You’re telling me we’ve advanced medicine to the point where we inject lab-made antibodies to fix what lifestyle and discipline should’ve prevented? People are obese, sedentary, and breathing polluted air - and now we pay $40k to patch the symptoms? This isn’t innovation - it’s surrender. If your asthma is this bad, maybe you should stop living in a city and start eating real food. Stop outsourcing your health to Big Pharma.
Eric Healy
November 24, 2025 AT 03:55They say omalizumab cuts attacks by 50 but what about the 50 who still get wrecked? And why do they always say "rare anaphylaxis" like it’s nothing? One in a thousand sounds safe until it’s your kid on the floor foaming at the mouth
Shannon Hale
November 25, 2025 AT 12:44OH MY GOD I WAS THE ONE WHO SAID THAT ABOUT BENRALIZUMAB AND JOINT PAIN 😭 I THOUGHT I WAS ALONE. I TOOK IT FOR THREE MONTHS AND FELT LIKE MY BONES WERE MELTING. I HAD TO QUIT. NO ONE LISTENS. I TOLD MY DOCTOR AND SHE JUST SMILED AND SAID "IT’S RARE." RARE? I’M THE ONE WHO LIVES IT. I STILL CAN’T REACH OVERHEAD. I HOPE THEY’RE LISTENING NOW.
Holli Yancey
November 27, 2025 AT 04:08I just wanted to say thank you for writing this. I’ve been scared to ask my doctor about biologics because I thought I wasn’t "sick enough." But reading this made me realize I’ve been surviving - not living. Maybe I’m a candidate. I’ll make the appointment this week.
Gordon Mcdonough
November 27, 2025 AT 18:01YOU THINK THIS IS BAD? WAIT TILL THEY START INJECTING AI-DESIGNED ANTIBODIES THAT LEARN YOUR ASTHMA TRIGGERS AND ADJUST IN REAL TIME. THEY’RE ALREADY TESTING IT. NEXT THING YOU KNOW - YOUR LUNGS WILL BE WIRED TO A CLOUD SERVER. THEY’RE TURNING HUMANS INTO BIO-ROBOTS. I’M NOT JOKING. THEY’RE USING YOUR DATA TO TRAIN THE NEXT GENERATION OF DRUGS. YOU’RE NOT A PATIENT - YOU’RE A DATASET.
Jessica Healey
November 29, 2025 AT 12:09My mom’s on Xolair and she cries every time she gets the shot because she’s so grateful. She used to be too scared to take the kids to the park. Now she chases them. I don’t care how much it costs - this is worth every penny. I just wish more people knew this was possible.