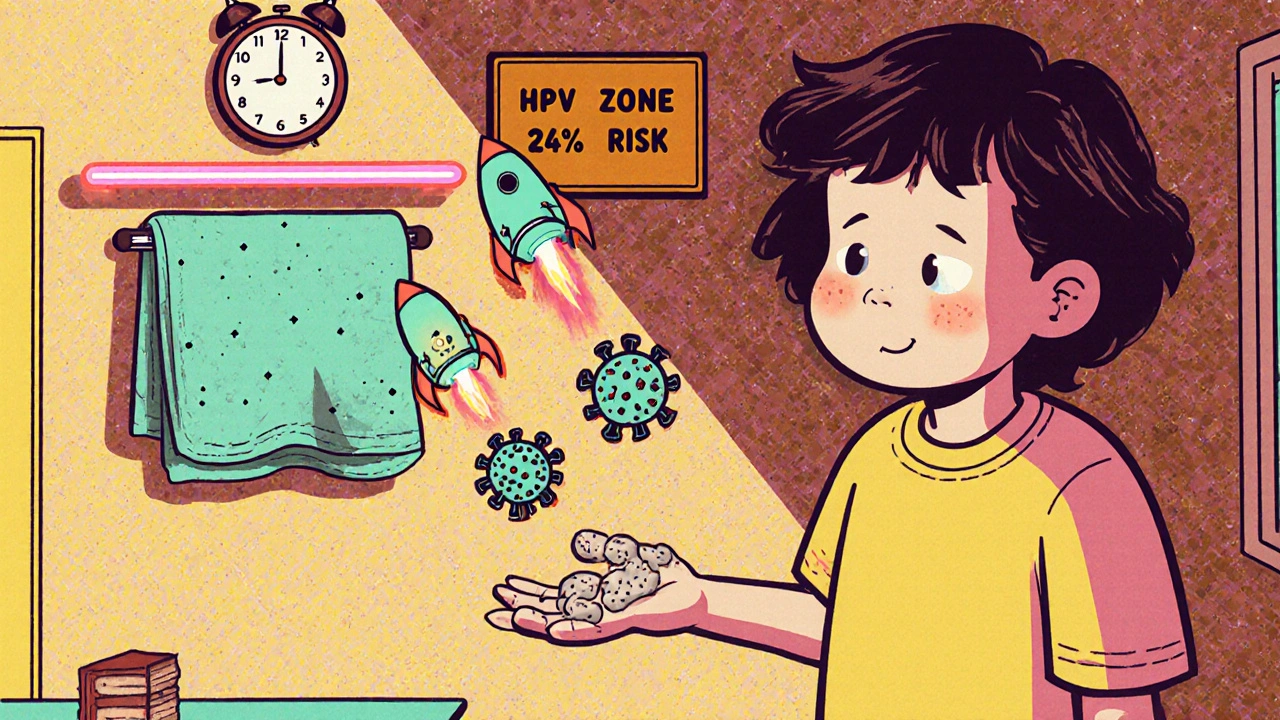
Most people think warts are just a nuisance - ugly bumps on the skin that won’t go away. But they’re not just cosmetic. Viral warts are caused by HPV, the human papillomavirus, and they’re far more common than you might think. In Australia, up to 24% of children and 5% of adults have them. Kids pick them up at school, adults get them from shared gym equipment or even barefoot walks in public showers. And while many warts disappear on their own - 60 to 70% within two years - most people don’t want to wait. They hurt. They spread. They embarrass.
What Causes Viral Warts?
Not all warts are the same. They’re caused by different strains of HPV, and each strain tends to show up in a specific spot. HPV is a family of over 100 viruses, and each one has a preferred target. For example:- Common warts (verruca vulgaris) usually show up on fingers, hands, or knees. They’re rough, raised, and often have tiny black dots - those are clotted blood vessels. HPV types 1, 2, and 4 are the usual suspects.
- Flat warts are smoother, smaller, and show up in clusters on the face, arms, or legs. They’re more common in kids and teens, and HPV types 3 and 10 cause them.
- Plantar warts grow on the soles of your feet. They’re often mistaken for calluses, but they hurt when you walk. HPV types 1, 2, 4, 60, and 63 are behind these. They grow inward because of pressure from walking, which makes them harder to treat.
HPV enters through tiny cuts or breaks in the skin. You don’t need to have a big wound - even a small scrape from a shoe or a hangnail can be enough. Once inside, the virus tricks skin cells into multiplying faster than normal, forming the wart. It’s not dangerous, but it’s contagious. You can spread it to other parts of your body or to other people through direct contact or shared towels, socks, or shower floors.
Why Don’t Warts Just Go Away?
Your immune system can handle HPV - eventually. That’s why so many warts vanish without treatment. But the process is slow. Some people wait months or even years. And while your body fights, the wart can spread. The virus hides in the deeper layers of the skin, where immune cells have a harder time finding it. That’s why some warts stick around for years, especially in people with weakened immune systems or those who keep reinfecting themselves by scratching or shaving over them.It’s not about being ‘dirty’ or ‘weak.’ It’s about biology. Some people’s immune systems just respond slower to HPV. That’s why two siblings might both touch the same towel, but only one gets warts.
Topical Treatments: What Actually Works?
If you’re trying to treat a wart at home, you’ve probably seen dozens of products on the shelf. But not all of them work. The two most proven options are salicylic acid and trichloroacetic acid.Salicylic acid is the gold standard for over-the-counter treatment. You can buy it in pads, liquids, or gels with concentrations between 17% and 40%. It works by slowly peeling away the infected skin. The key? Consistency. You need to apply it every day, soak the wart in warm water for 10 minutes first, then gently file away the dead skin with an emery board or pumice stone. Don’t share the file - it can spread the virus. Studies show an 84% success rate for plantar warts when used correctly over 6 to 12 weeks.
Trichloroacetic acid (TCA) is stronger and usually applied by a doctor. It burns the wart tissue on contact. Dermatologists often scrape the surface first to help the acid penetrate deeper. It’s especially useful for warts on thick skin, like the soles of feet or palms. Side effects include pain, burning, and sometimes dark spots on the skin. Scarring is rare if done properly.
Other acids - like glycolic, citric, or pyruvic - are sold online or in naturopathic stores, but there’s almost no solid evidence they work better than salicylic acid. Zinc creams and duct tape? Some people swear by them, but large studies haven’t proven they’re more effective than placebo.
In-Office Treatments: When Home Care Isn’t Enough
If warts don’t budge after 12 weeks of home treatment, it’s time to see a dermatologist. The two most common professional treatments are cryotherapy and electrosurgery.Cryotherapy uses liquid nitrogen to freeze the wart. It’s quick, widely available, and covered by most insurance plans. The doctor sprays it on for 10 to 20 seconds, freezing the tissue about 2-3mm beyond the visible edge. You’ll feel a sharp sting, then a burning sensation. The wart turns white, then blisters. It falls off in 1-2 weeks. Most people need 3 to 6 sessions, spaced 2 to 3 weeks apart. If you wait longer than 4 weeks between treatments, success drops from 75% to 40%. That’s a huge difference.
A 2023 review of seven studies involving nearly 1,000 patients found cryotherapy and salicylic acid had nearly identical success rates for common warts. Neither was clearly better. But when used together - salicylic acid at home, cryotherapy every few weeks - the cure rate jumped to 78%.
Electrosurgery burns the wart off with a tiny electric needle. It’s faster - often just one or two visits - but it leaves a small scar. It’s usually reserved for stubborn warts that haven’t responded to anything else. Laser treatment, like the VBeam pulse dye laser, targets the blood vessels feeding the wart. It’s effective but expensive and not always covered by insurance. The wart turns purple or black right after treatment and sloughs off in a week or two.
Surgical removal? Dermatologists avoid it. Cutting out warts often leads to more warts growing back around the scar. The virus is still in the surrounding skin.

Immunotherapy: Training Your Body to Fight Back
Sometimes, the problem isn’t the treatment - it’s your immune system. That’s where imiquimod comes in. It’s a cream that wakes up your skin’s immune cells and tells them to attack the HPV-infected tissue. It’s not a quick fix. You apply it three times a week for up to 16 weeks. You’ll see redness, swelling, and itching - that’s the immune system doing its job. But for warts that won’t respond to acid or freezing, imiquimod has a high success rate. One study showed it cleared warts that had resisted cryotherapy and salicylic acid.It’s not FDA-approved for non-genital warts in Australia, but dermatologists prescribe it off-label all the time. It’s especially useful for flat warts on the face or clusters of warts that keep coming back.
What Doesn’t Work - And Why
There’s a lot of noise out there. Cantharidin? Applied by doctors, it causes blisters. It works, but it’s messy and painful. Silver nitrate? Used for centuries, but studies show it’s no better than salicylic acid. Phenol? Risky - can damage nerves. Formic acid? Too weak. Most of these have been tried, but only a handful have solid data.The biggest myth? That warts are caused by frogs or toads. They’re not. HPV only infects humans. You can’t catch a wart from touching an animal.
How to Prevent Warts From Spreading
Treating the wart is only half the battle. Stopping it from spreading is just as important. Here’s what actually helps:- Don’t pick, scratch, or bite warts. You’re spreading the virus to other parts of your skin.
- Use separate towels, socks, and shoes. Wash them in hot water after each use.
- Wear flip-flops in public showers, pools, and locker rooms.
- Don’t share razors or nail clippers - HPV can hide in dead skin.
- Keep your skin moisturized. Dry, cracked skin is more likely to let HPV in.
- Boost your immune system with sleep, stress management, and good nutrition. It’s not a cure, but it helps your body fight faster.
When to See a Doctor
You don’t need to rush to a dermatologist for every little bump. But you should go if:- The wart is painful, bleeding, or changing color.
- It’s on your face, genitals, or around the nails.
- You have diabetes or a weakened immune system - you’re at higher risk for complications.
- It hasn’t improved after 12 weeks of home treatment.
- You’re not sure if it’s a wart or something else - melanoma can sometimes look like a wart.
Dermatologists can do a quick visual exam or, if needed, a biopsy to confirm it’s HPV. Don’t guess. Misdiagnosing a skin cancer as a wart can be dangerous.
Realistic Expectations
There’s no magic cure. Every treatment - whether it’s acid, freezing, or cream - takes time. Most require multiple visits or weeks of daily use. Side effects like pain, redness, and scarring are possible. And even after the wart disappears, the virus might still be there. Recurrence rates are around 20-30% within a year.That’s why patience and consistency matter more than speed. The goal isn’t to zap it in one day. It’s to outlast the virus.
And remember - even if you’ve had warts before, you’re not doomed. Many people clear them permanently after one successful treatment. Others need a few tries. Either way, you’re not alone. Millions of Australians deal with this every year. The key is knowing what works, avoiding the hype, and sticking with a plan.
Are viral warts contagious?
Yes. Viral warts are caused by HPV, which spreads through direct skin contact or shared objects like towels, shoes, or gym equipment. You can also spread them to other parts of your own body by scratching or shaving over them.
Can I treat warts at home safely?
Yes, with salicylic acid products. Apply daily after soaking and gently filing the wart. Avoid using them on the face, genitals, or if you have diabetes or poor circulation. Never mix home treatments with professional ones without consulting a doctor.
How long does cryotherapy take to work?
Most people need 3 to 6 sessions, spaced 2 to 3 weeks apart. Each session takes less than a minute. The wart usually falls off 1 to 2 weeks after freezing. Waiting longer than 4 weeks between treatments reduces success rates by nearly half.
Do warts come back after treatment?
Yes, in about 20-30% of cases. The virus can linger in nearby skin even after the wart is gone. That’s why hygiene and immune health matter. Recurrence is more common in people with weakened immune systems or those who don’t complete treatment.
Is there a vaccine for non-genital warts?
The HPV vaccines (Gardasil 9, Cervarix) protect against strains that cause genital warts and cervical cancer, but not the types that cause common or plantar warts. So while they’re important for sexual health, they won’t prevent warts on your hands or feet.
What’s the most effective treatment for plantar warts?
Studies show salicylic acid and cryotherapy are equally effective. Combining both - daily acid at home and professional freezing every 2-3 weeks - gives the best results, with cure rates up to 78%. Avoid surgery; it often leads to more warts around the scar.

shreyas yashas
November 22, 2025 AT 00:39I used to have a plantar wart that lasted 18 months. Tried duct tape, apple cider vinegar, you name it. Nothing worked until I started salicylic acid daily, soaked my foot, filed it down, and stuck with it. No magic, just consistency. Now it’s gone and I don’t even miss it.
Also, never share your pumice stone. I learned that the hard way - ended up with three more on my other foot.
Suresh Ramaiyan
November 23, 2025 AT 20:35It’s wild how something so common gets so much stigma. People act like warts are a sign you’re unclean or weak. But it’s just biology - some immune systems take longer to catch up. My kid got flat warts on his forehead from school, and we didn’t do anything for a year. They vanished. No treatment needed. Just patience.
And yeah, HPV is everywhere. We’re all walking around with it. The body’s usually way smarter than we give it credit for.
Katy Bell
November 25, 2025 AT 19:51Okay but can we talk about how terrifying it is to see a wart on your kid’s face? I cried. Not because it was ugly - because I thought it was skin cancer. Took me two weeks to finally take her to the derm. Turns out? Just flat warts. Thank god.
Imiquimod was a nightmare though. Red, itchy, swollen - she screamed every time I put it on. But it worked. And now she’s wart-free. Worth it.
Linda Rosie
November 26, 2025 AT 11:17The most effective treatment for plantar warts is a combination of salicylic acid and cryotherapy, with a cure rate of up to 78% when used together. This is supported by peer-reviewed clinical studies from 2023.
Vivian C Martinez
November 27, 2025 AT 09:38So many people panic when they see a bump on their skin. But honestly? If it’s not bleeding, changing shape, or hurting - just wait. Your body’s got this. I had a wart on my finger for three years. One day, poof. Gone. No treatment. Just time.
Don’t stress. Stress makes your immune system worse anyway.
Ross Ruprecht
November 28, 2025 AT 20:56Ugh I hate when people act like warts are some big mystery. It’s just a virus. Use salicylic acid or get it frozen. Done.
Why are we writing essays about this? Just fix it.
Bryson Carroll
November 29, 2025 AT 06:23Everyone’s so obsessed with ‘natural remedies’ and ‘boosting immunity’ like it’s a yoga retreat. Newsflash - HPV doesn’t care if you drink green tea or sleep 8 hours. It’s a virus that multiplies in keratin. Salicylic acid dissolves it. Cryo burns it. Everything else is placebo with a marketing budget.
And no - duct tape is not a treatment. It’s a cry for help from someone who’s read too many blog posts.
Lisa Lee
November 30, 2025 AT 08:50Why is this even a thing in the US? In Canada we just cut them off and move on. No 12-week waiting games. No ‘boost your immune system’ nonsense. We’ve got good doctors. We use the tools. Problem solved.
Also - stop wearing flip-flops in showers. Wear socks. It’s 2025.
Jennifer Shannon
December 2, 2025 AT 01:24Have you ever thought about how warts are kind of like emotional baggage? They stick around because we ignore them, then we panic when they spread… and then we try every solution under the sun, hoping for a miracle?
But really - it’s just your body trying to tell you something. Maybe you’re stressed. Maybe you’re not sleeping. Maybe you’ve been walking barefoot in that locker room since college and never thought twice.
Salicylic acid works? Sure. But so does taking a breath. So does washing your feet. So does not picking at it. Healing isn’t just about chemicals - it’s about rhythm. Routine. Respect for your own skin.
I had a wart for four years. I didn’t treat it. I just started wearing socks to bed. I moisturized. I stopped scratching. And one morning - it was gone. No cryo. No acid. Just… me, being gentle.
Maybe that’s the real treatment. Not the science. The silence.
Also - I’m not saying don’t use the acid. I’m saying: don’t rush the process. Let your body catch up. It’s been holding on longer than you think.
Suzan Wanjiru
December 3, 2025 AT 13:07Plantar warts are the worst because they hurt when you walk. I used to limping around like I had a stone in my shoe. Salicylic acid worked but only after I started soaking my feet in Epsom salt first - softens the skin so the acid penetrates better.
Also - file the wart after every soak. Don’t skip that step. It’s the key. And never use the same emery board on your nails - I learned that the hard way.
My dermatologist said cryo is fine but you gotta do it every 2 weeks. Wait longer and it’s useless. I did 5 sessions. Gone in 10 weeks.
Don’t waste money on zinc creams or garlic. It’s snake oil.
Kezia Katherine Lewis
December 3, 2025 AT 19:05It’s important to note that the HPV strains implicated in cutaneous warts (e.g., HPV-1, HPV-2, HPV-4) are phylogenetically distinct from those associated with mucosal lesions (e.g., HPV-6/11). Consequently, the current quadrivalent and nonavalent HPV vaccines confer no cross-protection against non-genital cutaneous manifestations. This is a critical distinction often conflated in public discourse.
Additionally, while imiquimod is used off-label for non-genital warts, its mechanism involves TLR7 agonism, which upregulates IFN-alpha and IL-12, thereby enhancing dendritic cell-mediated antigen presentation - a key immunomodulatory pathway that is often underutilized in primary care settings.
Henrik Stacke
December 5, 2025 AT 03:09As someone who grew up in the UK, I can confirm that the NHS used to offer cryotherapy for warts on the NHS until they stopped - cost-benefit analysis, apparently. Too many people turning up with stubborn warts, too few resources.
So now? They hand you a tube of salicylic acid and say ‘try this for 12 weeks’. It’s frustrating, but honestly? It works. I’ve seen it.
And yes - don’t share towels. We’re not animals. It’s basic hygiene. Even if you’re in a rush, just hang your towel on a hook. It’s not hard.
Manjistha Roy
December 6, 2025 AT 17:49My sister had a wart on her knee for five years. She tried everything. Then one day she just stopped touching it. No treatment. No panic. And it disappeared. Not because of medicine - because she stopped stressing about it.
Stress weakens your immune system. That’s the real secret. Not the acid. Not the freezing. Just letting go.
Also - never use a razor over a wart. You’ll spread it everywhere. I speak from experience.
And please stop believing in ‘natural cures’ from Instagram. Salicylic acid is science. Everything else is noise.
Jennifer Skolney
December 6, 2025 AT 20:29Just wanted to say - if you’re reading this and you’re embarrassed about your warts? You’re not alone. I had them on my fingers for two years. I wore gloves in summer. I hid my hands.
Then I started salicylic acid. It burned. It itched. I cried a few times. But I stuck with it.
And now? I wear tank tops. I don’t hide.
You got this 💪
JD Mette
December 7, 2025 AT 08:29I used to think warts were just a kid thing. Then I got one on my heel after a trip to the gym. Didn’t think much of it. Took me 14 months to finally do something about it.
Salicylic acid worked. But only because I didn’t give up. I soaked. I filed. I reapplied. Every day. No excuses.
Also - I started wearing socks to bed. Weird, I know. But it kept me from scratching in my sleep.
It’s not glamorous. But it works.
Suresh Ramaiyan
December 7, 2025 AT 16:45What’s interesting is how some people’s bodies just ignore HPV for years - then suddenly, boom, immune system wakes up and clears it. Like your skin had a nap and woke up mad.
That’s why I don’t panic anymore. I just watch. Wait. Let the body do its thing. Sometimes the best treatment is doing nothing - with patience.