Pregnancy Hypertension Medication Checker
Check if your blood pressure medication is safe during pregnancy and get recommendations for pregnancy-safe alternatives.
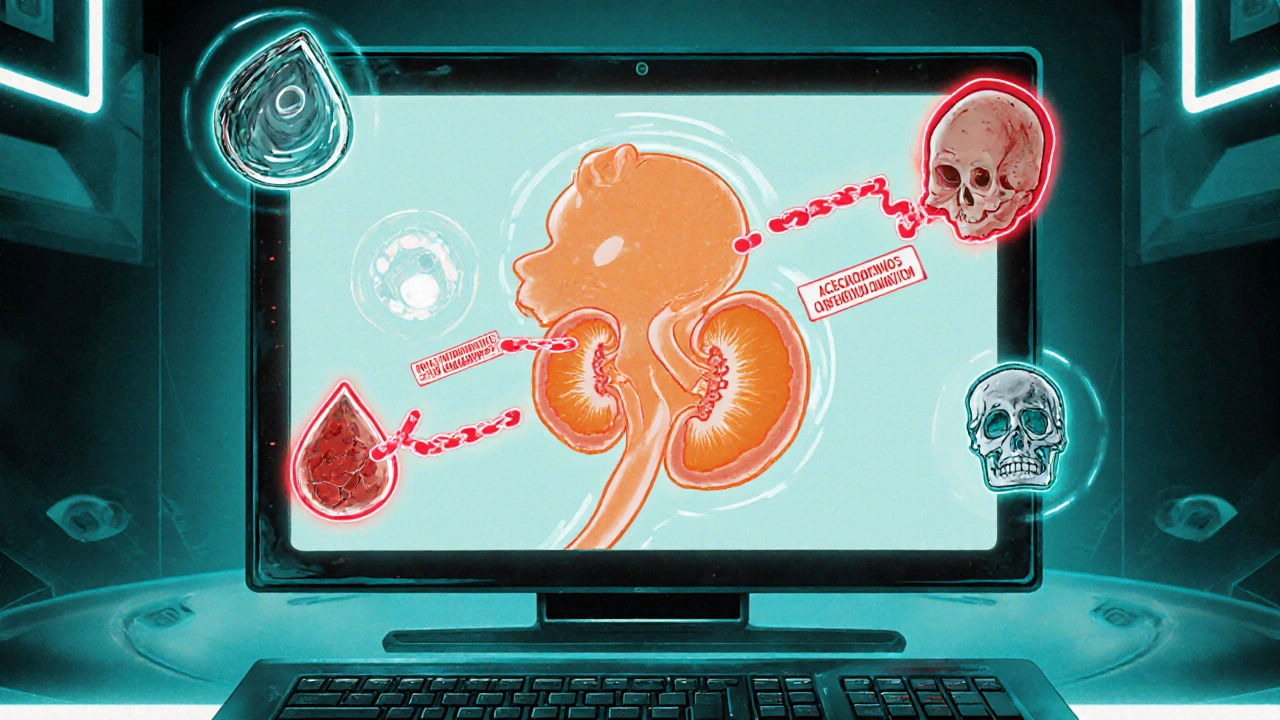
Finding out you’re pregnant while you’re on blood‑pressure pills can feel like a heart‑stopper. The good news? There are clear guidelines and safe alternatives, and the bad news? Certain drugs - especially pregnancy risk of ACE inhibitors and ARBs - can seriously harm a developing baby.
Why ACE Inhibitors and ARBs Are Off‑Limits
ACE inhibitors are a class of antihypertensive drugs that block the enzyme that turns angiotensin I into the powerful vasoconstrictor angiotensin II. By lowering angiotensin II, they relax blood vessels and drop blood pressure. ARBs (angiotensin II receptor blockers) work a step downstream, stopping angiotensin II from binding to its receptor. Both families are fantastic for most adults, but during pregnancy they interfere with the baby's renin‑angiotensin system - a system that’s essential for kidney formation and amniotic fluid production.
When that system gets blocked, the most common fetal complications are:
- Fetal renal damage
- Oligohydramnios (too little amniotic fluid)
- Skull deformities
- Severe hypotension and hyperkalaemia
- Neonatal renal failure or death
Studies consistently show higher miscarriage rates, lower birth‑weight averages (about 350 g less), and shorter gestations (roughly 1.8 weeks earlier) in pregnancies exposed to these drugs.
What the Guidelines Say
The American College of Obstetricians and Gynecologists (ACOG) “Practice Bulletin No. 234” (2022) instructs clinicians to stop ACE inhibitors and ARBs as soon as pregnancy is confirmed - no matter the trimester. The American Heart Association (AHA) echoes this in its 2023 Presidential Advisory, labeling the exposure as “fetal renin‑angiotensin system blockade syndrome.”
Regulators back the medical societies. The Food and Drug Administration (FDA) still carries a Category D boxed warning for all ACE inhibitors and ARBs, stating clear evidence of fetal risk. The European Medicines Agency and New Zealand’s Medsafe have identical warnings.
How Big Is the Problem?
Even with these warnings, medication‑error data from the FDA’s 2021 adverse‑event reports show that about 1.2 % of pregnancies in women with chronic hypertension still involve an ACE inhibitor or ARB. That translates to several thousand affected pregnancies each year in the United States alone.
Why does it happen? Often because women of child‑bearing age aren’t asked about pregnancy plans before a prescription is written, or they aren’t aware that the drug is unsafe during pregnancy.
Safe Alternatives for Managing Hypertension in Pregnancy
When pregnancy is confirmed or planned, clinicians switch to antihypertensives with a long safety record. The top three options are:
- Labetalol - a combined alpha‑ and beta‑blocker that’s first‑line for most pregnant patients. Starting dose is usually 100 mg twice daily, titrated up to 2,400 mg/day.
- Methyldopa - a centrally acting alpha‑2 agonist with the longest pregnancy safety record (since the 1970s). Typical dosing begins at 250 mg twice daily, maxing at 3 g/day.
- Nifedipine - a calcium‑channel blocker used as second‑line, especially when blood pressure spikes suddenly. Immediate‑release tablets start at 10 mg three times daily.
All three aim for a target blood pressure of < 140/90 mmHg in uncomplicated pregnancies. They are far less likely to cause oligohydramnios or fetal renal injury.
Side‑by‑Side Comparison
| Drug Class | Typical Example | Pregnancy Category (US) | Major Fetal Risks | Usual Use in Pregnancy |
|---|---|---|---|---|
| ACE Inhibitor | Lisinopril | D | Renal failure, oligohydramnios, fetal death | Contraindicated - stop immediately |
| ARB | Losartan | D | Higher rates of neonatal complications than ACEIs | Contraindicated - stop immediately |
| Beta‑blocker/Alpha‑blocker | Labetalol | B | Generally safe; rare fetal bradycardia | First‑line antihypertensive |
| Alpha‑2 Agonist | Methyldopa | B | Well‑studied safety; mild sedation possible | First‑line, especially early pregnancy |
| Calcium‑Channel Blocker | Nifedipine | C | Safe in most cases; watch for cardiac output drop in heart disease | Second‑line, acute severe hypertension |
Practical Steps for Clinicians and Patients
- Ask every woman of child‑bearing potential about pregnancy plans before prescribing any antihypertensive.
- If pregnancy is possible, choose a Category B or C drug (labetalol, methyldopa, nifedipine) rather than an ACE inhibitor or ARB.
- When a patient becomes pregnant while on an ACEI/ARB, stop the drug immediately and switch to a safe alternative within 24‑48 hours.
- Monitor blood pressure twice weekly in the first trimester, then weekly thereafter; adjust dosing as needed.
- Perform ultrasound assessments of amniotic fluid volume at 20 weeks to catch early oligohydramnios.
- Provide counseling on reliable contraception if the patient wishes to stay on an ACE inhibitor or ARB for another condition (e.g., heart failure) and is not planning pregnancy.
These steps reduce the odds of fetal injury and keep maternal blood pressure under control.

What Happens If Exposure Occurs Late in Pregnancy?
Exposure during the second or third trimester is the most dangerous. The fetus’s kidneys are actively forming, and blocking the renin‑angiotensin system can cause severe renal hypoplasia. In practice, neonates may be born with fetal renal damage that requires dialysis or prolonged hospital stays. Oligohydramnios can also lead to lung compression, increasing the risk of respiratory distress after birth.
If a late‑pregnancy exposure is identified, the obstetric team typically coordinates a detailed fetal ultrasound, assesses amniotic fluid index, and prepares for possible neonatal intensive care. Early delivery may be considered if the fetus is near term and the risk of continuing the pregnancy outweighs prematurity concerns.
Key Takeaways for Expectant Mothers
- Never start or continue an ACE inhibitor or ARB once you’re pregnant.
- Ask your doctor to switch you to labetalol, methyldopa, or nifedipine as soon as pregnancy is confirmed.
- Regular prenatal visits and blood‑pressure checks are essential for a healthy pregnancy.
- If you’re planning to conceive, discuss medication changes before trying.
Frequently Asked Questions
Can I take an ACE inhibitor in the first trimester?
No. Even though early‑trimester exposure might not cause major structural defects, it still raises the risk of miscarriage, lower birth weight, and later kidney problems. Guidelines advise stopping the drug as soon as pregnancy is known.
Why are ARBs considered riskier than ACE inhibitors?
ARBs block the receptor directly, which can produce a more complete shutdown of the fetal renin‑angiotensin system. Studies show higher rates of neonatal complications and mortality with ARBs compared to ACE inhibitors.
What is the safest blood‑pressure target during pregnancy?
Most guidelines recommend keeping systolic below 140 mmHg and diastolic below 90 mmHg unless you have pre‑eclampsia or other complications, in which case tighter control may be needed.
If I was on an ACE inhibitor before I got pregnant, do I need to switch right away?
Yes. Stop the ACE inhibitor immediately and start a pregnancy‑safe alternative such as labetalol or methyldopa under your doctor’s guidance.
Can breastfeeding mothers use labetalol?
Labetalol is considered compatible with breastfeeding. Small amounts pass into milk, but studies show no adverse effects on infants.
Bottom line: ACE inhibitors and ARBs are a clear no‑go for any stage of pregnancy. Switch early, monitor closely, and use a proven, pregnancy‑safe antihypertensive. Talking openly with your healthcare team will keep both you and the baby healthy.


Jennifer Stubbs
October 25, 2025 AT 13:12ACE inhibitors and ARBs pose a clear danger to fetal kidney development and amniotic fluid balance, which can lead to serious neonatal outcomes. The pharmacologic blockade of the renin-angiotensin system interferes with essential renal morphogenesis during the second and third trimesters. Clinical data show a consistent rise in miscarriage rates and a measurable drop in birth weight when these drugs are used during pregnancy. Regulatory agencies such as the FDA, EMA, and Medsafe have all issued boxed warnings that reflect the seriousness of the risk. Even though the agents are effective for adult hypertension, their safety profile changes dramatically in the gestational environment. ACOG’s practice bulletin explicitly instructs physicians to discontinue ACE inhibitors and ARBs as soon as pregnancy is confirmed, regardless of gestational age. The alternative antihypertensives-labetalol, methyldopa, and nifedipine-have been studied for decades and demonstrate a far more favorable fetal safety record. Labetalol’s combined alpha and beta blockade provides steady blood pressure control without compromising renal perfusion. Methyldopa’s long history of use dates back to the 1970s, offering reassurance about its teratogenic profile. Nifedipine, as a calcium‑channel blocker, is useful for acute spikes and is generally well tolerated in pregnancy. Monitoring protocols should include bi‑weekly blood pressure checks in the first trimester, progressing to weekly assessments later on. Ultrasound evaluation of amniotic fluid volume around 20 weeks can catch early signs of oligohydramnios. Patient counseling about contraception is essential for women who may need to stay on ACE inhibitors or ARBs for non‑pregnancy indications. Switching to a pregnancy‑safe regimen should be done within 24‑48 hours of pregnancy detection to minimize fetal exposure. In cases where exposure occurs later in gestation, a detailed fetal ultrasound and preparation for possible neonatal intensive care are warranted. Early delivery may be considered if the fetus is near term and the risk of continued exposure outweighs prematurity concerns. Ultimately, the goal is to protect both maternal health and fetal development by using drugs with proven safety in the pregnant population.
Abby W
October 27, 2025 AT 19:45Wow, thanks for breaking all that down 🙌 It's crazy how many people still end up on the wrong meds 🤦♀️ If you ever feel unsure, just double‑check with your OB and ask for a switch to something like labetalol or methyldopa 🙏 Stay safe out there!
the sagar
October 30, 2025 AT 03:18Stop trusting any pharma lies about ACE inhibitors-they're a weapon against our babies.
Grace Silver
November 1, 2025 AT 10:52The interplay between maternal hypertension and fetal renal development invites us to reflect on the delicate balance of life
we must honor the science while also listening to the lived experiences of pregnant women seeking safe care
Clinton Papenfus
November 3, 2025 AT 18:25Esteemed colleagues it is incumbent upon us to uphold the highest standards of clinical practice by eschewing contraindicated agents during gestation and embracing proven alternatives with due diligence.
Zaria Williams
November 6, 2025 AT 01:58okay so like i read thru all that and i gotta say its pretty spot on but also u know some doctors still mess up lol just gotta keep pushin for better patient edu 🤷♀️
Tamara Tioran-Harrison
November 8, 2025 AT 09:32Indeed, the suggestion to simply "switch" without acknowledging the systemic inertia of pharmaceutical lobbying is delightfully naive 😏. One might suggest a comprehensive overhaul of prenatal prescribing guidelines, but that would be far too ambitious for a single comment.
kevin burton
November 10, 2025 AT 17:05For anyone needing a quick summary: stop ACE inhibitors/ARBs if pregnant, use labetalol, methyldopa, or nifedipine instead, and keep blood pressure under 140/90 with regular check‑ups.