PID Risk Assessment Tool
This tool estimates your risk of developing Pelvic Inflammatory Disease (PID) based on your symptoms and infection history. PID is an infection of the upper genital tract that can follow untreated vaginal infections.
Results are for informational purposes only. Please consult a healthcare provider for proper diagnosis and treatment.
Your PID Risk Assessment
What to do next:
Quick Takeaways
- PID is an infection of the upper genital tract that can follow untreated vaginal infections.
- Common vaginal infections that raise PID risk include bacterial vaginosis, trichomoniasis, chlamydia and gonorrhea.
- Symptoms of PID often overlap with lower‑tract infections, making early diagnosis tricky.
- Prompt treatment with antibiotics and safe‑sex practices dramatically lower the chance of long‑term damage.
- If you notice pelvic pain, fever, or unusual discharge, see a health professional right away.
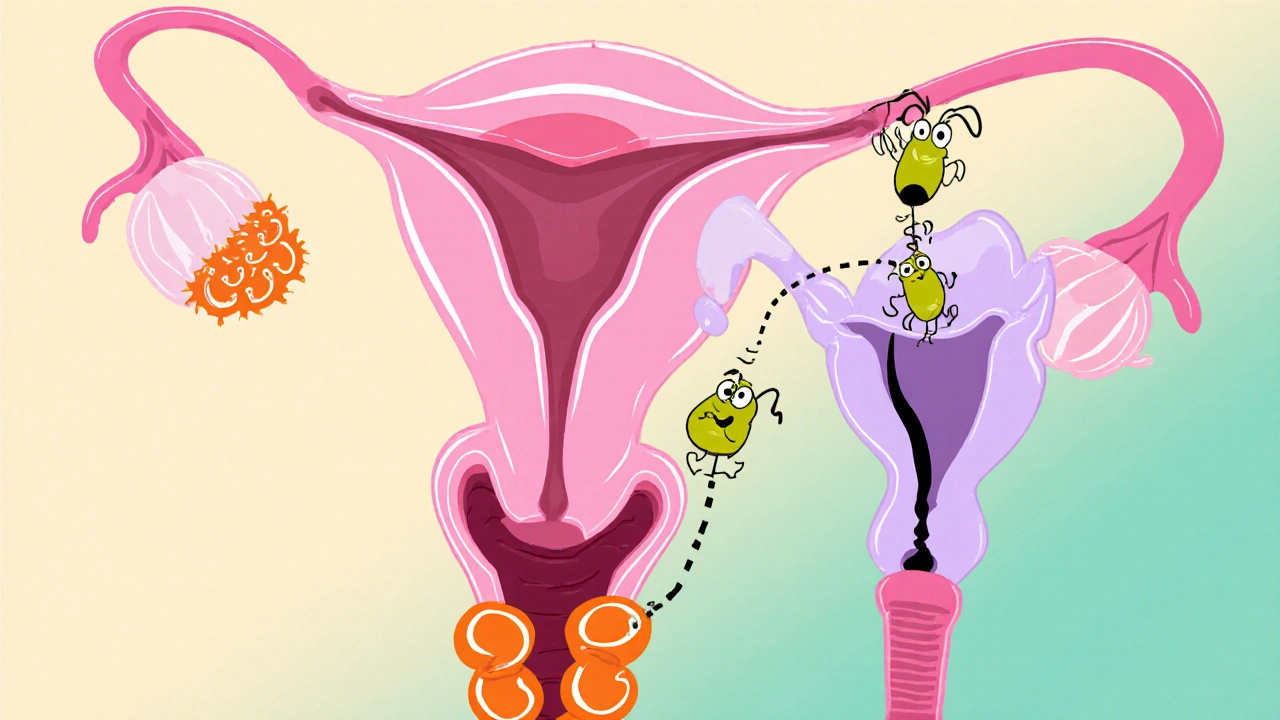
When a Pelvic Inflammatory Disease is described as an infection of the uterus, fallopian tubes, and nearby pelvic organs, many people wonder how a problem that starts in the vagina can travel upward. The answer lies in the anatomy of the female reproductive system and the way certain microbes exploit it. This guide explains the link, points out the infections that matter most, and shows you how to spot and stop the cascade before it turns into a serious health issue.
What Is Pelvic Inflammatory Disease?
pelvic inflammatory disease (PID) is a broad term for inflammation and infection of the upper genital tract. It usually begins when bacteria ascend from the lower genital tract into the uterus, fallopian tubes, or ovaries. If left untreated, PID can cause chronic pelvic pain, infertility, ectopic pregnancy, or tubo‑ovarian abscesses.
Typical PID signs are lower‑abdominal or pelvic pain, abnormal vaginal bleeding, fever, and a foul‑smelling discharge. However, up to 70% of cases present with mild or no symptoms, which is why understanding risk factors-especially vaginal infections-is crucial.
How Vaginal Infections Set the Stage
A vaginal infection is any imbalance of the normal flora or invasion by harmful microorganisms in the lower genital tract. When the protective barrier is disrupted, bacteria gain easier access to the cervix and then the uterus.
Two main mechanisms drive this upward spread:
- Ascending Pathway: Pathogens travel up the mucous membrane, especially during menstruation or after intercourse when the cervical os is slightly open.
- Inflammatory Facilitation: Some infections trigger inflammation that loosens tight junctions between cells, making it easier for bacteria to slip through.
Not every vaginal infection leads to PID, but several have a documented link.

Vaginal Infections With the Highest PID Risk
The table below compares the most common infections, their classic symptoms, and how likely they are to seed PID.
| Infection | Typical Symptoms | PID Risk | Standard Treatment |
|---|---|---|---|
| Bacterial Vaginosis | Thin gray‑white discharge, fishy odor, mild itching | Medium - alters vaginal pH, making ascent easier | Metronidazole 500mg PO BID 7days |
| Trichomoniasis | Yellow‑green frothy discharge, itching, burning | Medium - inflammation of the cervix can aid bacteria | Metronidazole 2g PO single dose |
| Candidiasis (Yeast Infection) | Thick white “cheese‑like” discharge, intense itching | Low - primarily fungal, not bacterial | Fluconazole 150mg PO single dose |
| Chlamydia trachomatis | Often asymptomatic; may cause mild discharge | High - most common bacterial cause of PID | Doxycycline 100mg PO BID 7days |
| Neisseria gonorrhoeae | Purulent discharge, burning urination | High - frequently leads to PID when untreated | Ceftriaxone 500mg IM + Azithromycin 1g PO |
Notice that sexually transmitted infections (STIs) such as chlamydia and gonorrhea sit at the top of the risk ladder. Even infections that are not classic STIs-like bacterial vaginosis-can change the vaginal environment enough to invite more aggressive bacteria.
Symptoms Overlap: Why PID Is Hard to Spot Early
Both vaginal infections and PID can cause abnormal discharge, pelvic discomfort, and urinary symptoms. The key differences often lie in the location and intensity of pain:
- Lower‑tract infection: Discomfort is usually limited to the vulva or vagina; pain improves with emptying the bladder.
- PID: Pain is deeper, constant, and may worsen with movement, coughing, or during intercourse.
- Fever, chills, or a feeling of being “very sick” leans toward PID.
Because many women dismiss mild pelvic pain as “period cramps,” it’s easy for PID to slip by until complications arise.
How Doctors Diagnose PID
Diagnosis starts with a thorough history and pelvic exam. Doctors look for cervical motion tenderness, adnexal tenderness, and uterine tenderness-collectively known as the “CHAMPS” criteria.
Laboratory tests can confirm the underlying infection:
- NAAT (nucleic acid amplification test) for Chlamydia and Gonorrhea.
- Microscopic exam (wet mount) for Trichomoniasis.
- A Gram stain or culture for bacterial vaginosis.
Imaging-usually transvaginal ultrasound-helps identify tubo‑ovarian abscesses or fluid collections that indicate severe PID.

Treatment Pathways and Prevention
Effective treatment hinges on two goals: eradicate the offending microbes and stop the spread to the upper genital tract.
- Antibiotic regimens: CDC recommends a combination of doxycycline plus a single‑dose cephalosporin for broad coverage.
- Partner therapy: Treating sexual partners prevents reinfection, especially for chlamydia and gonorrhea.
- Follow‑up: Re‑evaluation 48‑72hours after starting therapy ensures fever resolution and symptom improvement.
Prevention strategies focus on maintaining a healthy vaginal microbiome and reducing STI exposure:
- Limit douching-it disrupts normal flora and raises BV risk.
- Use condoms consistently; they cut PID‑causing STI transmission by over 50%.
- Get screened annually for chlamydia and gonorrhea if you’re sexually active under 25 or have new partners.
- Consider probiotic supplements containing Lactobacillus crispatus after a course of antibiotics.
When to Seek Care Immediately
If you notice any of the following, call a health professional right away:
- Sudden, severe pelvic or lower‑abdominal pain.
- Fever≥38°C (100.4°F) with pelvic discomfort.
- Foul‑smelling, greenish, or bloody discharge.
- Painful urination accompanied by pelvic tenderness.
Early intervention cuts the risk of infertility and chronic pain dramatically.
Frequently Asked Questions
Can a yeast infection cause PID?
Yeast infections are fungal and usually stay in the lower tract. They rarely lead to PID, but they can coexist with bacterial infections that do. Treating any candidiasis alongside bacterial vaginosis ensures the whole ecosystem stays balanced.
Is bacterial vaginosis considered an STI?
BV is not classified as an STI, but sexual activity can shift the vaginal pH, making BV more common in sexually active women. It still raises PID risk by altering the protective acid barrier.
How long does it take for untreated chlamydia to cause PID?
Chlamydia can ascend within weeks, but many women remain asymptomatic for months. Studies show up to 20% of untreated chlamydia cases develop PID within 3months.
Can I self‑treat a vaginal infection to avoid PID?
Over‑the‑counter products may relieve itching, but they won’t eradicate bacterial causes like BV or chlamydia. A proper diagnosis and prescription antibiotics are essential to stop the infection from moving upward.
Is it safe to have sex while being treated for PID?
Abstinence or consistent condom use is recommended until the full antibiotic course is finished and symptoms have resolved. This prevents re‑infection and protects the partner.

Nicola Gilmour
October 15, 2025 AT 12:23Hey everyone, just wanted to say that staying on top of vaginal health is a huge win for your overall wellness-think of it like a daily power‑up for your body! By catching an infection early you can dodge the nasty cascade that leads to PID, and that means less worry, less pain, and more energy for the things you love. Keep up with regular check‑ups, use condoms consistently, and don’t shy away from talking to your doctor if something feels off. You’ve got the tools-use them and stay strong!
Darci Gonzalez
October 16, 2025 AT 16:10Got the gist? Treat those infections fast 😊 it stops the bad guys from climbing up the tract and keeps you feeling great.
Marcus Edström
October 17, 2025 AT 19:56It’s worth noting that the ascending pathway isn’t just a theoretical concept-it’s observed in clinical studies where untreated chlamydia or gonorrhea directly precede PID in a sizable fraction of cases.
kevin muhekyi
October 18, 2025 AT 23:43PID is no joke.
Teknolgy .com
October 20, 2025 AT 03:30Interesting read, but let’s not pretend the table covers every nuance 😒 there are emerging pathogens that slip through the cracks and the guide leaves them out.
Caroline Johnson
October 21, 2025 AT 07:16Wow!!!, this article really nails the key points, but, seriously, where’s the discussion on antibiotic resistance, which is, frankly, a huge oversight, especially considering the rise of multidrug‑resistant gonorrhea, and, don’t even get me started on the lack of patient‑centric follow‑up protocols!!!
Megan Lallier-Barron
October 22, 2025 AT 11:03While many celebrate routine screenings, I’d argue that over‑screening can lead to unnecessary anxiety and overtreatment, especially when asymptomatic chlamydia often resolves without medical intervention-just think about the cascade of side effects from antibiotics.
Kelly Larivee
October 23, 2025 AT 14:50Bottom line: keep your vagina’s pH balanced, use condoms, and see a doc if you notice any weird discharge.
Emma Rauschkolb
October 24, 2025 AT 18:36From a microbiome perspective, dysbiosis-characterized by a depletion of Lactobacillus spp. and overgrowth of anaerobes-creates a permissive environment for opportunistic pathogens to ascend, culminating in PID 😷. Early intervention restores eubiosis and mitigates systemic inflammatory cascades.
Kaushik Kumar
October 25, 2025 AT 22:23First and foremost, the prevention of PID starts with education, which empowers individuals to recognize the subtle signs of lower‑tract infections before they evolve into something more serious.
Second, consistent condom usage acts as a physical barrier, dramatically lowering the transmission rates of chlamydia and gonorrhea, the two pathogens most frequently implicated in PID.
Third, routine screening-particularly for sexually active people under the age of 25-allows for the early detection of asymptomatic infections, which might otherwise linger unnoticed.
Fourth, when an infection is identified, adherence to the full antibiotic course is crucial; stopping treatment prematurely can lead to bacterial persistence and resistance.
Fifth, partner treatment eliminates the source of reinfection, a step that many patients neglect, thereby re‑exposing themselves to the same pathogens.
Sixth, lifestyle modifications, such as avoiding douching, help maintain the natural acidic environment of the vagina, which is a key defense mechanism against pathogenic overgrowth.
Seventh, probiotic supplementation after antibiotics can re‑populate the vaginal flora with beneficial Lactobacillus strains, supporting long‑term microbial balance.
Eighth, clinicians should employ the CHAMPS criteria during pelvic exams; cervical motion tenderness, uterine tenderness, and adnexal tenderness together provide strong diagnostic cues.
Ninth, if imaging is indicated, transvaginal ultrasound offers a non‑invasive way to assess for tubo‑ovarian abscesses or fluid collections, guiding further management.
Tenth, patients experiencing fever, severe pelvic pain, or a foul‑smelling discharge should seek immediate medical attention, as these are red‑flag symptoms for advanced PID.
Eleventh, public health initiatives that promote STI awareness and destigmatize testing play a pivotal role in reducing the overall burden of PID within communities.
Twelfth, research continues to explore novel antimicrobial regimens that target resistant strains, underscoring the importance of staying up‑to‑date with evolving treatment guidelines.
Thirteenth, interdisciplinary collaboration between gynecologists, primary care physicians, and infectious disease specialists ensures comprehensive care for affected individuals.
Fourteenth, patient education materials should be culturally sensitive and linguistically appropriate to maximize outreach and comprehension across diverse populations.
Finally, by integrating these strategies-education, prevention, early detection, proper treatment, and follow‑up-we can dramatically cut down the incidence of PID and safeguard reproductive health for generations to come.
Mara Mara
October 27, 2025 AT 01:10Hello friends! As a proud advocate for our nation's health, I must stress that protecting women from PID is a patriotic duty-our communities thrive when families stay healthy, and that starts with smart choices like regular screenings and barrier protection!!!
Jennifer Ferrara
October 28, 2025 AT 04:56It is with the greatest due reverence that I commence this discourse; the cognizant reader shall note that whilst the chronicle herein is thorough, occasional mispells such as "etymology" instead of "etymology" may enigmatically arise, yet they do not detract from the perspicuity of the presented facts.
Terry Moreland
October 29, 2025 AT 08:43Really appreciate the detail here. It helps to know what to watch for and how to act fast. Simple steps like using condoms and getting checked can make a huge difference.
Abdul Adeeb
October 30, 2025 AT 12:30Allow me to point out a few grammatical observations: the phrase "lower‑tract infections" should be hyphenated, and the verb "lead" in the opening sentence must agree with its plural subject "infections". Additionally, consistency in the usage of the Oxford comma throughout the list would enhance readability.